Home >
Erectile Dysfunction >
Adenomectomy for prostate cancer
Adenomectomy for prostate cancer
Surgical treatment of prostate cancer
Radical treatment
The optimal method of treatment of Prostate cancer localized in the prostate gland is its radical removal along with the gland. The effectiveness of radical prostatectomy in relation to the life expectancy of patients and the duration of the period of absence of clinical signs of the disease is determined by the timely operation before the spread of the malignant process to the paraprostatic tissue, seminal vesicles and the development of distant metastases. Radical prostatectomy can not only eliminate the focus of malignancy, but also prevent local recurrence of prostate cancer. At the same time, many urologists are in favor of less radical alternative treatments for localized prostate cancer - remote c-therapy, interstitial nuclide implantation, or a combination of these methods. The preference for radiotherapy is justified by the lower incidence of complications associated with its use. However, experience indicates the advantage of radical prostatectomy over radiation therapy in achieving complete removal of the primary focus of prostate cancer. At the same time, the frequency of complications with these two treatments does not differ significantly.
The main criteria in evaluating indications for radical prostatectomy are the detection of histological signs of prostate cancer in more than 10% of tissue sections obtained during transurethral resection or adenomectomy; histological signs of carcinoma in a biopsy specimen of a focal dense prostatic node obtained by needle biopsy; normal activity of the prostatic fraction of acid phosphatase in the blood, no signs of bone metastases according to X-ray and nuclide studies; the general good condition of the patient, allowing for surgery. Currently, the generally accepted point of view is that the success of radical prostatectomy depends on the anatomical spread of prostate cancer.
The tactics of surgical treatment is determined by the stage of prostate cancer. Thus, Prostate cancer stages T0a and T0b are tumors of intraglandular localization, which are accidentally detected in the tissue of remote adenomatous nodes. Prostate cancer stages T0a and T0b are classified into focal microscopic (signs of malignancy are detected in less than 3 tissue sections of removed adenomatous nodes) and diffuse microscopic (signs of malignancy are detected in more than 3 tissue sections of removed adenomatous nodes). Focal microscopic prostate cancer in most cases refers to tumors of a high degree of differentiation, has an extremely weak biological growth potential, and therefore the likelihood of recurrence of the primary tumor and the development of distant metastases is very low.
Removal of focal microscopic prostate cancer with adenomatous nodes is the same radical operation as total prostatectomy, if the surgeon is sure that this clinical stage of the disease is correctly determined and that the process does not spread to the gland capsule and seminal vesicles. According to pelvic lymphangioadenography, there are no metastases in the pelvic lymph nodes in focal microscopic prostate cancer.
Diffuse-microscopic prostate cancer (stage T0b), in contrast to focal-microscopic (stage T0a), is characterized by an active biological potential, and most of the tumors at this stage, according to the histological structure, belong to prostate cancer of a moderate or low degree of differentiation, which is combined with metastases in the pelvic lymph nodes. In this regard, the indications for radical prostatectomy for stage T0b prostate cancer should be evaluated carefully, the operation is advisable only if a well-differentiated tumor is detected, in which the likelihood of metastases in the pelvic lymph nodes is minimal. In these cases, immediate radical prostatectomy is indicated after the detection of latent prostate cancer in the prostate tissue obtained by transurethral resection or adenomectomy. Patients with prostate cancer of stages T1 and T2 (stage B according to classification A-D), making up 10 - 20% of all patients with adenocarcinoma of the prostate, are the main contingent for radical prostatectomy.
The curability of prostate cancer after radical prostatectomy according to the life expectancy of patients, the duration of remission and recurrence of the primary tumor is largely determined by the clinical stage, the histological structure of the tumor and the presence of metastases in the pelvic lymph nodes.
Prostate cancer stages T1 and T2 (B1 and B2) is a palpable tumor localized in the gland.At the same time, from the point of view of determining the indications for radical prostatectomy, it is important to consider the features of tumors of this type according to their size, histological differentiation, the likelihood of invasion of the seminal vesicles and metastases in the pelvic lymph nodes. Thus, an important difference between stage T1a prostate cancer (a solitary node less than 1.5 cm in size, palpable in one of the lobes of the gland) and T1b (a palpable seal in one of the lobes of the gland with a diameter of more than 1.5 cm) is a lower probability of invasion of the seminal vesicles and extracapsular spread of the malignant process. The frequency of metastases in regional lymph nodes in stages T1a and T1b is extremely low in well-differentiated tumors (about 4%) and increases as the cancer dedifferentiates (up to 33%). This gives reason to consider radical prostatectomy indicated for patients with clinical stages T1a and T1b, which can be performed without prior pelvic lymphadenectomy in cases of a well-differentiated histological type of cancer. In prostate cancer stages T1a and T1b of moderate and low degree of differentiation, a combination of pelvic lymphadenectomy and radical prostatectomy is necessary to improve the results of surgical treatment due to the increased likelihood of metastases in the pelvic lymph nodes. Stage T2 prostate cancer is a large tumor nodule larger than 2 cm in diameter, occupying most of one lobe of the gland, with the possibility of spreading to the adjacent area of the gland. Prostate cancer stage T2 of low differentiation is accompanied by a high frequency of metastases in the lymph nodes, which determines the inappropriateness of radical prostatectomy in patients of this category. At the same time, the frequency of metastases of prostate cancer stage T2 in the pelvic lymph nodes is 18 - 27%. In these cases, pelvic lymphadenectomy makes it possible to identify patients with no metastases in the lymph nodes, which greatly expands the indications for radical prostatectomy. In patients with stage T2 prostate cancer with no metastases in the pelvic lymph nodes, microscopic invasion of the gland capsule and seminal vesicles is minimal, which gives grounds to predetermine a good prognosis of radical prostatectomy. Thus, radical prostatectomy at stage T2 is justified in cases of a truly localized tumor focus in the gland, the removal of which makes it possible to achieve a life expectancy of patients of 10–15 years. Stage T3 prostate cancer usually extends beyond the capsule of the gland and has a high rate of lymph node metastases (about 50%), as well as a low degree of histological differentiation. In this regard, radical prostatectomy is not advisable at this stage.
Radical prostatectomy is most indicated for patients with localized prostate cancer that has not spread beyond the capsule of the gland and in the absence of signs of distant metastases (stages T1 - T2). The life expectancy of patients with prostate cancer of these stages, subjected to radical prostatectomy, corresponds to the life expectancy of healthy men of the same age. The accumulated clinical experience indicates a 5-, 10-, and 15-year survival rate in patients with stage T1-2 prostate cancer subjected to radical prostatectomy. The probability of duration of remission and life expectancy increases in the absence of signs of penetration of the capsule and microscopic spread of the malignant process to the seminal vesicles according to the histological examination of the removed gland with seminal vesicles adjacent to it ("surgical" block). It should be noted that the microscopic infiltration of the capsule by malignant cells, revealed during the histological examination of the "surgical" block, does not increase the risk of recurrence of prostate cancer in the absence of microscopic invasion of the seminal vesicles. Detection of microscopic invasion of the seminal vesicles in the remote "surgical" block increases the likelihood of local recurrence of prostate cancer and the development of distant metastases.
The goal of radical prostatectomy is the total removal of the prostate gland as a single unit with the bladder neck and seminal vesicles. The need for this is determined by multicentricity, which is a characteristic feature of the development of prostate cancer. The results of transurethral resection or hormone therapy in patients with stage T1-2 prostate cancer are significantly worse than those of radical prostatectomy. There are also no convincing data on the advantages of radiation therapy over radical prostatectomy in the treatment of localized prostate cancer.The results of radiation therapy and radical prostatectomy are difficult to compare, since during radiation therapy a very small number of patients undergo pelvic lymphadenectomy, and it is not possible to obtain information on the degree of involvement of the lymph nodes, gland capsule and seminal vesicles in the malignant process. Along with this, the interpretation of the results of histological studies of tissue biopsies of the irradiated prostate gland, which retained a residual tumor, is still quite controversial. At the same time, radiation therapy is the preferred treatment for prostate cancer of clinical stages T0b and T2 in the presence of a large cancer node and low histological differentiation of the tumor due to the high probability of invasion of the seminal vesicles and metastases in the pelvic lymph nodes.
Radical prostatectomy can be performed by perineal and retropubic access. Before perineal radical prostatectomy, pelvic retroperitoneal lymphadenectomy (through a lower median laparotomy) is preliminarily performed as an independent operation. The advantages of perineal prostatectomy are a good view during anastomosis of the reconstructed bladder neck with the membranous part of the urethra, a lower risk of surgical bleeding than with retropubic prostatectomy. In perineal radical prostatectomy, the anastomosis of the bladder neck and urethra is formed by suturing their edges over a 24 Foley catheter inserted into the urethra. 4 sutures are applied - on the anterior, posterior and lateral surfaces of the anastomosis.
Retropubic prostatectomy is a large-scale operation, and the main problem in its implementation is the prevention of operative and postoperative bleeding. Reconstruction of the bladder neck and reanastomosis of the bladder with the urethra are technically difficult. Surgical and postoperative bleeding during retropubic prostatectomy can be minimal when taking into account the topographic and anatomical relationship of the dorsal vein of the penis and the Santorini venous plexus. To prevent bleeding, it is recommended to ligate the dorsal vein of the penis prior to the intersection and ligation of the puboprostatic ligaments. This significantly reduces bleeding during the operation and improves the conditions for creating an anastomosis between the bladder neck and the membranous part of the urethra after removal of the prostate and seminal vesicles. The formation of the cervical-urethral anastomosis is completed by placing 4 sutures on each quadrant of the anastomosis circumference over the 24 Foley catheter inserted into the urethra
Complications associated with radical prostatectomy are classified as intraoperative, early, and late postoperative. Complications during surgery include rectal perforation, damage to the ureters and bleeding.
Rectal perforation is more common with perineal prostatectomy (10%) than with retropubic (4%). The perforation hole in the intestine is sutured during the operation with two-layer sutures. Prevention of this complication is a thorough preoperative preparation, especially in diseases of the rectum. Transurethral resection and radiation therapy performed before radical prostatectomy increase the risk of perforation of the rectal wall.
Another surgical complication is dissection of the ureters. Pre-insertion of ureteral catheters after opening the bladder reduces the risk of damage to them. At the same time, despite the preliminary introduction of ureteral catheters, the ureters can be damaged when large seminal vesicles are released. Careful and thorough isolation is important to prevent damage to the juxtavesical segments of the ureters. If the ureters are damaged during perineal radical prostatectomy, then their reconstruction is carried out by perineal access through the open bladder neck. The integrity of the ureters damaged during retropubic prostatectomy is restored by their reanastomosis.
Excessive blood loss is one of the formidable complications of radical prostatectomy. To reduce it, it is recommended to mobilize the urethra at the apex of the prostate gland by dissecting the puboprostatic ligaments near the place of their transition to the periosteum of the pubic bone, as well as tearing the pelvic fascia away from its border, extending along the prostate gland. These measures make it possible to safely ligate the deep dorsal vein of the penis before it flows into the Santorini venous plexus.
Early postoperative complications include impaired renal function, cardiovascular and thromboembolic complications (myocardial infarction, pulmonary embolism, thrombophlebitis), wound infection, lymphocele, pelvic hematoma.
The pathogenesis of acute transient renal ischemia is associated with large blood loss. An additional factor in the development of anuria may be a hematoma that compresses the urinary tract. The formation of a hematoma in the deep parts of the pelvis increases the risk of developing thrombophlebitis and pulmonary embolism.
Hemodynamic disturbances due to acute blood loss create prerequisites for the development of myocardial infarction. Improvement in surgical technique and careful hemostasis during radical prostatectomy have reduced the incidence of these complications.
The formation of lymphocele (cysts in the retroperitoneal space filled with lymph) in the early postoperative period after pelvic lymphadenectomy and radical prostatectomy is 4 - 5%. The mechanism of their development is associated with dissection during pelvic lymphadenectomy of efferent lymphatic vessels with subsequent accumulation of lymph in the retroperitoneal space. Predisposing factors are previous radiation therapy, prolonged treatment with corticosteroids, diuretics, the presence of a metastatic tumor in the lymph nodes, hematoma in the pelvic cavity, infection. Lymphocele can be unilateral or bilateral. Clinically, pelvic lymphoceles are asymptomatic or manifest as symptoms of compression of the organs to which they are adjacent (ureters, bladder, rectosigmoid segment, iliac vessels). Most often, these are symptoms of compression of the ureters, irritation of the bladder, stool retention, swelling of the genital organs, pain in the lower abdomen, and swelling of the legs. The diagnosis is established on the basis of excretory urography, cystography, CT and echography of the pelvis. To prevent a lymphocele during lymphadenectomy, it is necessary to carefully ligate the edges of the resected lymphatic vessels. Treatment of a lymphocele is to aspirate the contents of the cyst, followed by drainage. In some cases, it is necessary to resort to excision of the cyst with suturing the edges of its wall to the abdominal wall to fill the cavity with lymphocele granulations. Additionally, antibiotics and anticoagulants are used.
Late complications of radical prostatectomy include urinary incontinence, urethral stricture, and contracture of the bladder neck.
Urinary incontinence after radical prostatectomy is 2 - 5%. For the prevention of lymphocele during lymphadenectomy, a carefully sparing nature of the operation is necessary, especially when manipulating the pelvic diaphragm, which is closely related to the function of the external sphincter of the bladder.
Narrowing in the area of the vesicourethral anastomosis is manifested by symptoms of urinary retention with the presence of a large volume of residual urine. In this case, there is a need to perform transurethral resection of the stenosing vesicourethral junction. With the development of urethral stricture distal to the vesicourethral anastomosis, bougienage or internal urethrotomy is performed.
So, radical prostatectomy is an effective treatment for localized prostate cancer. Improving methods for diagnosing the stages of prostate cancer, histological gradation of the tumor and metastases in the pelvic lymph nodes makes it possible to identify patients with localized prostate cancer and more widely use radical prostatectomy for their treatment.
Adenomectomy of the prostate
Surgical intervention is one of the methods for treating prostate pathologies, in particular, removal of neoplasms in the gland.
Adenomectomy is an operation that is performed when a man develops prostate adenoma (a benign formation in the prostate gland). The procedure is a complete removal of a growing neoplasm.
In what cases is the operation assigned
Surgical intervention is resorted to in cases where there is an active increase in the number of atypical cells in the gland. This usually happens if the pathology is discovered late, or the patient did not adhere to the medical recommendations of his attending physician earlier.
There are a number of typical symptoms and conditions of the patient that indicate the growth of the neoplasm and require adenomectomy.
- Gland enlargement;
- A sharp deterioration in urodynamic parameters;
- Difficulty urinating;
- Frequent outbreaks of urological inflammatory diseases (cystitis, urethritis);
- Renal failure, usually chronic.
Contraindications
- Previously performed adenomectomy;
- Prostate cancer;
- Adhesions in the pelvic organs;
- A pronounced inflammatory process in the body;
- Pathologies of the heart;
- Diabetes mellitus.
Important! The possibility of performing an operation on the prostate is determined by the attending physician, based on a comprehensive diagnosis of the patient.
Types of operation
Surgical removal of an adenoma is carried out according to different methods. Operations differ from each other in how the affected prostate is accessed and how it is removed.
Among the applied types of adenomectomy are:
- Posterior pubic - open surgery on the prostate, in which the bladder is not affected;
- Transvesical - abdominal surgery, in which the tumor is removed through the bladder;
- Transurethral (TUR) is the most common and gentle method, used for small neoplasms.
Preparing for surgery
Important! 8 hours before the adenomectomy, the patient should refrain from eating and drinking.
No additional preparatory procedures are required.
Immediately before the operation, the patient is examined by an anesthesiologist. This is necessary to determine the appropriate method of anesthesia. Open prostate surgery can be performed under general or epidural anesthesia, depending on the complexity of the disease and the individual patient's parameters.
How does adenomectomy work
The course of the operation depends on which of the adenomectomy techniques is used:
- Posterior pubis. The surgeon makes an incision in the lower abdomen, from the navel down to the pubic bone. Having parted the tissues and bypassed the bladder, the doctor discovers the affected gland. The tumor is removed and sutures are applied;
- Overbubble. The cut is made in the same way. Next, the walls of the bladder are cut, and through its cavity, the doctor gains access to the adenoma, removes it and stitches the tissues;
- Transurethral. Minimally invasive endoscope treatment. The device is installed in the urethra, visualizes the adenoma and removes neoplasms.
Advantages and disadvantages of adenomectomy
The disadvantage of surgical intervention for prostate adenoma is:
- long and difficult rehabilitation period after open surgery;
- high chance of complications;
- a large number of contraindications.
Advantages of different adenomectomy techniques:
- Retropubic: the prostate is in a position of direct visibility, but the bladder remains intact - this reduces the risk of surgical injuries and their consequences;
- Transvesical: the operation with the highest efficiency. Allows you to treat adenoma in the most complex form;
- Transurethal: minimal surgical intervention, the entire procedure is carried out through a special monitor. This type of surgery has the least chance of complications.
Possible complications after surgery
Complications during adenomectomy can be divided into two groups:
- appearing directly during the operation;
- postoperative.
During the procedure itself, the following negative consequences may occur:
- TUR syndrome (or water intoxication syndrome). During the operation, the bladder is irrigated with special solutions, as a result of which an excess amount of fluid enters the blood vessels;
- Surgical damage to the urethra, which in the future may provoke a deterioration in the functioning of the gland (including the performance of sexual function);
- Poor blood clotting or destruction of the integrity of the blood vessel, resulting in severe bleeding;
- Infection in the prostate gland and the development of the inflammatory process;
- Allergy to anesthetic.
Postoperative complications after adenomectomy include:
- Incontinence or retention of urine. Occurs due to changes in the muscle tissue of the bladder;
- Retrograde ejaculation - sperm after ejaculation enters the bladder, and not out.
Rehabilitation period
At the end of the operation, the patient is transferred to the hospital and stays there until the sutures are completely healed. The average duration is from 7 to 10 days.
Photo 2: During this period, it is recommended to avoid spicy and fatty foods, preferring protein foods and fiber. Source: flickr (Eugene Evehealth).
For the period of rehabilitation, the patient may be prescribed medications:
- antibiotics - to prevent infection and inflammation;
- painkillers - to relieve discomfort.
It's important to know! In the first few days after surgery, blood will appear in the patient's urine - this is normal. Urination during this period is controlled by a doctor.
After an adenomectomy, the patient is advised to maintain moderate activity - you can walk and move, but do not overdo it. Return to a full-fledged rhythm of life and physical activity is possible not earlier than 5-7 weeks after the operation.
Removal of a prostate tumor by surgical methods: consequences
According to statistics, prostate cancer is one of the most diagnosed diseases in men.
It can affect people of all ages, and the mortality rate from this disease is in third place.
About the disease
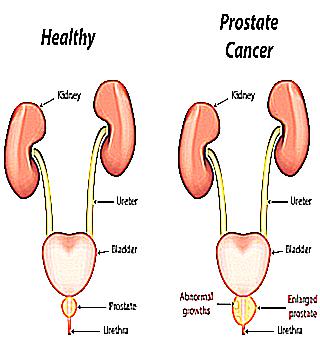
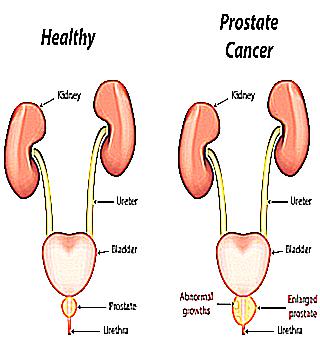
Prostate cancer (prostate) is a malignant neoplasm that arises from the tissues of the prostate glands due to changes in prostate cells in DNA. Modern medicine still does not know the exact causes of prostate cancer. You can read more about this here.
Some factors that increase the risk of developing a tumor can be identified:
Age. Over the years, the likelihood of developing a tumor increases. It is extremely rare for men in the age group under 40 to get sick, after 50 the possibility of the disease is growing every year. Heredity. The probability of acquiring prostate cancer is higher in men who have relatives with such a disease (if there are sick blood relatives, the risk of developing the disease increases by 8 times). Nutrition. Excessive consumption of animal fats promotes tumor formation. In overweight men, prostate cancer is detected more often. Smoking. Tobacco smoke contains cadmium, which contributes to the development of prostate cancer. Ultraviolet radiation. Contains in its composition vitamin D3, which inhibits the movement of cell growth. In the oncological structure of many countries, prostate cancer ranks 2-3, behind stomach and lung cancer.
The disease tends to appear in mature men (after 40-50 years), after 60-70 years its frequency increases.
Approximately 40% of men of this age have latent (hidden) prostate cancer, and only in 10% of cases the latent form begins to manifest itself as a clinical picture and can lead to death.
A distinctive feature of prostate cancer is characterized by its slow development, due to the absence of symptoms at the initial stage.
Treatment options
It takes about 2-3 years for localized prostate cancer to double in size. At the same time, it is able to remain within the gland.
A common way to treat prostate cancer is radiation therapy (X-ray therapy) - a method of treating malignant tumors with the help of ionizing radiation. Cancer cells multiply much faster than ordinary cells, and radiation from radiation therapy disrupts cell division and DNA synthesis.
The advantage of X-ray therapy is the absence of a surgical operation for a prostate tumor in men, the disadvantage is the inability to control the development of the tumor throughout life. According to studies, after the use of radiation therapy, the ability to maintain a normal level of the substance in the cells of the prostate is only 10%. After surgery - 70%.
Other treatment options for prostate cancer:
Chemotherapy is the treatment of cancer with drugs to reduce the growth of cancer cells while also affecting healthy cells. This hormone therapy lowers testosterone levels and slows down the course of the disease. Immunotherapy is a technique based on the use of drugs that activate the immune system. Weak cancer cells are introduced into the body, and the immune system begins to destroy them, mistaking them for foreign cells. High Intensity Focused Ultrasound Ablation is a method in which tissues are heated with intense ultrasound and tumor cells are damaged. Side effects from this procedure are minimal. Often, in the formation of prostate cancer, doctors use complex treatment, combining chemotherapy with radiation.
Radical removal of the prostate: what is it? Radical removal of the prostate is the most common operation to remove the prostate gland (for oncology). Its goal is to remove the tumor within healthy fields, and maintain control over urinary functions and sexual activity. Surgery for prostate cancer is performed on people whose cancer has not spread to neighboring organs.
Doctors, when prescribing therapy by the method of surgery, rely on the ability of each organism to withstand surgery, which is a serious procedure. This procedure has become the most popular in the treatment of prostate cancer, because without eliminating the disease it is radically impossible to control its transition to neighboring organs.
And if this happened, cancer cannot be cured and cannot be stopped. In the presence of bone metastases, the expected life expectancy is no more than 3 years.
The absolute indications for prostate removal are:
- stopped prostate cancer (stages 1 and 2) in the absence of metastases and regional lymph nodes;
- obstruction of the urinary tract (difficulty in passing urine) associated with stage 3 prostate cancer;
- an advanced form of prostate adenoma that is not amenable to other treatment, which is rare.
Removal of the prostate for cancer and consequences
How to remove the prostate? There are several ways to remove prostate cancer. Radical prostatectomy is considered more effective.
Radical prostatectomy is an operation to remove prostate cancer, performed for localized disease. It is the main method of treatment with preservation of urinary function and erectile function.
When performing an operation to remove prostate cancer, great skill of the doctor is required, because along the edges of the prostate there are sphincters of the urethra and small nerves responsible for erection, which must be preserved.
Complex therapy is often used after prostatectomy, combining radiation and hormonal treatment.
In addition to radical prostatectomy, there are several more modern surgical methods for removing the prostate gland:
Transurethral resection of the prostate (TUR). The safest method of removal, carried out in mild forms of the disease, when the kidneys are not damaged, and the bladder is able to empty. TUR is painless.
Surgery for prostate cancer involves inserting a thin endoscopic instrument into the urethra called a resectoscope.
When exposed to it, the prostate gland is removed and the blood vessels are coagulated. The prostate removal operation is carried out under general anesthesia or spinal anesthesia, and only in the case when the volume of the prostate gland does not exceed 80 ml.
The likelihood of complications is determined by the duration of the operation. Possible complications include bleeding, penetration of the urethral lavage fluid into the vascular bed.
TUR can not be performed with exacerbation of diabetes mellitus, disorders in the cardiovascular and respiratory systems, the use of drugs that thin the blood. Open adenomectomy. It is used in severe forms of diseases, when the prostate gland reaches large volumes, there is no emptying of the bladder, there is kidney failure.
It is also used for complications of prostate adenoma in the form of bladder stones. Surgery for a prostate tumor is open and traumatic.
Open adenomectomy requires general anesthesia or regional anesthesia. During the operation of removing the prostate, an incision is made in the bladder, presenting the affected area of the prostate to the doctor's gaze. A catheter should be placed in the bladder to drain the fluid.
For young men, prostate adenomectomy is fraught with a violation of potency. Open adenomectomy is not used in cases of concomitant serious diseases with a threat to life. Transurethral incision of the prostate (TUIP). The operation takes place in the presence of frequent or difficult urination, inability to empty the bladder completely, regular inflammatory diseases of the urinary tract, with a small prostate.
The procedure allows you to improve the outflow of urine and eliminate the manifestations of prostate adenoma.
Surgery is performed under general anesthesia or spinal anesthesia. A resectoscope with a knife at the end is inserted into the urethra. The surgeon makes two incisions in the prostate without excising the tissue.
Complications after TUIP are sexual disorders in the form of retrograde ejaculation. The operation is contraindicated for large prostates.
Complications
Removal of the prostate in men provides instant relief that lasts for years.
But such an extreme measure in treatment has a high risk of unwanted complications after prostate cancer surgery - consequences:
Rehabilitation
Despite the good health of the patient after the operation to remove the prostate, the body will take a long time to fully recover.
Rehabilitation after prostate cancer surgery:
In the first postoperative week, you need to be extremely careful, avoid sudden movements and leave physical exercises until better times; during the recovery period, you need to drink plenty of water to flush the bladder, about 8 glasses a day, this will speed up recovery; try to strain less during bowel movements; it is not allowed to lift weights during the recovery period, as well as driving a car; do not forget about the prescribed diet to prevent constipation (if it occurs, you need to consult a doctor about taking laxatives); with normal healing of the incision, the sutures are removed from it on the 9-10th day, after which you can take a shower (the possibility of taking baths, visiting the pool after prostate cancer surgery should be discussed with your doctor). To prevent the recurrence of prostate cancer after radical prostatectomy, you should visit a urologist at least once a year and undergo a digital rectal examination.
After removing the prostate, you can forget about the disease for up to 15 years. In some cases, repeated surgery is required. If you follow the medical recommendations, undergo the necessary procedures and timely visits to the doctor, life expectancy can be increased.
A tumor of the prostate gland can appear in any man. The main thing is not to miss the moment and diagnose the disease in time. Modern medical technologies allow in most cases to defeat the disease and continue to enjoy life.