ADS:
Azithromycin Vs Cephalexin: What's The Difference?
Having the appropriate antibiotic can aid in both treating bacterial infections and speeding up their healing process. Various infections are treated with antibiotics, including Azithromycin and Cephalexin. Despite their distinct categories and mechanisms of action, there are some common ground points between the two drugs that make choosing difficult.
The treatment of respiratory tract infections like bronchitis, pneumonia, sinusitis (infected with leukemia), and otitis media is often achieved by using Azithromycin, which is also a macrolide antibiotic. Cellulitis, erysipelases, and folliculitis are among the skin infections that can be treated with it. The antibiotic cephalexin, which is a first-generation cepharyngitis and tonsillitis product, is commonly used to treat UTIs, skin infections (UTIs), skin and soft tissue infections, pharyngitis, and tonsils.
Both medications have been extensively studied for their safety profiles and efficacy against various bacterial strains. They share similarities but exhibit notable differences in pharmacokinetics, dosage forms, and side effects as well as contraindications. Identifying the disparities is crucial in determining which antibiotic would be most effective for any particular infection or patient group.
Tablets or suspensions are the usual method of administration for Azithromycin, whereas Cephalexin is sold in oral form as either an oral capsule/liquid suspension. While Azithromycin typically has a shelf life of 3 to 5 days, Cephalexin is often prescribed for an extended period, lasting between 7 and 14 days.
Both antibiotics exhibit resistance profiles, which is their main difference. The activity of Azithromycin has been observed in specific strains of macrolide-resistant bacteria, such as MRSA. On the flip side, Cephalexin is not capable of killing MRSA and may be less effective against specific enterococci or anaerotic bacteria.
Comparing Azithromycin vs Cephalexin requires careful consideration of these factors alongside individual patient characteristics, such as age, weight, and any pre-existing medical conditions. Severe kidney disease may result in crystalluria if given along with Cephalexin. On the other hand, Cephalexin has a higher incidence of side effects but is generally well-absorbed.
Through an examination of the specific characteristics, benefits, and drawbacks of each antibiotic used by healthcare providers, doctors can develop more precise diagnoses and prescribe drugs that are most effective for their patients. By examining the mechanisms of action, indications, dosages, and contraindications for each, as well as the differences between Azithromycin and Cephalexin in treating different types of infections with various antibiotics such as crackers or levulcans (a zimper), we'll be able to advise you on which one to use.
Azithromycin vs Cephalexin
In the quest to combat bacterial infections, two popular antibiotics have emerged as frontrunners - Azithromycin and Cephalexin. Though their mechanisms of action are similar in some ways, the two drugs differ significantly (see pharmacokinetics, spectrum of activity (30 mg/kg; Side effect profiles (3), and recommended doses) for different infections. This comparison aims to provide clinicians with information on the benefits and drawbacks of each antibiotic, making them more knowledgeable about their effectiveness.
Broad-spectrum antibiotics are capable of killing gram-positive bacteria, including Streptococcus pneumoniae, HaEmophilus influenza, and Moraxella catarrhalis; they include the broad spectrum: Azithromycin is a macrolide antibiotic. The MAC that causes pulmonary infections in individuals with compromised immune systems is effectively targeted by this organism. Unlike its counterpart, Cephalexin is an early-stage cephalosporin that targets predominantly gram-positive bacteria, such as Staphylococcus aureUS and Streptozoozotococcuses (Streptoccobacteria) pyogenes and some strains of Haemophilus influenzae.
In contrast to its plasma half-life of 12-14 hours, Azithromycin exhibits a distinct pharmacokinetic profile with extended functional half lives in tissues for up to 2-3 days. By allowing for frequent dosing (once or twice daily) and improving persistence within phagocytic cells, this feature facilitates the removal of intracellular pathogen species. In contrast, Cephalexin has a shorter lifespan in the tissue (4-6 hours), necessitating frequent dose adjustments (proband therapy) every 2-3 hours.
Azithromycin and Cephalexin are typically more easily absorbed, with reduced incidences of gastro-intestinal problems and hypersensitivity reactions. In some cases, the use of azithromycin can lead to QT interval prolongation, which is a rare but serious problem that can increase the risk of torsades de pointes in patients with pre-existing cardiac conditions or those receiving concurrent medications known as extended QTR. Although it is commonly tolerated, CephalexIN exposure may result in gastrointestinal discomfort and occasionally anaphylaxis.
Different azithromycin dosages are recommended for different indications. In cases of community-acquired pneumonia (CAP), it is common to receive a 5-day course of 500 mg orally once daily, which is usually enough. Cephalexin is a medication that can be taken at doses of 250-500 mg every 6 hours for 7-14 days, in contrast to other options such as skin and soft tissue infections or urinary tract infections.
Due to its extended half-life, broad-spectrum activity against gram-positive and intracellular pathogens, and improved tolerability, Azithromycin is well-suited for treating respiratory infections such as COPD (bacterium communis). The effectiveness of Cephalexin in treating skin and soft tissue infections, as well as urinary tract infections, is due to its ability to kill common gram-positive pathogens at the infection site.
Understanding Antibiotic Differences
Understanding their variations is essential when selecting an antibiotic for treatment. Antibiotics have varying properties that make them more effective against specific infections. In this section, we'll delve into the key factors that set antibiotics apart and help you better understand their distinct features.
- Antibiotics are classified by their chemical structure or mechanism of action. For instance, macrolides like azithromycin target bacterial protein synthesis, while cephalosporins such as cephalexin inhibit cell wall formation.
- Antibiotics have varying levels of effectiveness against different types of bacteria. Azithromycin is a broad-spectrum antibiotic that targets gram-positive and some gram-negative pathogens, while cephalexin is focused on killing primarily Gram-negative organisms such as Staphylococcus aureus and Streptococcus pneumoniae.
- Resistance patterns: Antibiotic-resistant strains are becoming increasingly prevalent. Cephalosporins face more challenging challenges than cephalons, which have less stability in developing resistance. Azithromycin has shown greater stability to date.
- Dosing schedules and bioavailability of antibiotic drugs vary based on the recommended dosages. For a period of five days, it is possible to take Azithromycin orally for one dose per day, while cephalexin needs to be given twice daily for seven to ten days.
- Patients may exhibit varying reactions to different antibiotics due to differences in their pharmacokinetic and metabolic characteristics, leading to different side effect profiles. The most common side effects of Azithromycin include gastrointestinal distress and allergic reactions, while cephalexin can cause diarrhea, nausea, or skin irritation.
By grasping these fundamental differences between azithromycin and cephalexin, you'll be better equipped to make an informed decision when selecting the most appropriate antibiotic for your specific infection. The next section will examine the two medications and compare them directly using this knowledge.
Mechanism of Action Explained
Azithromycin and cephalexin are both antibiotics that work by interfering with the bacteria's ability to make proteins, which are essential for their growth and survival. Interference occurs at different points in the process of bacteria generating proteins.
- The ribosome, where amino acid chains are assembled, is targeted by Azithromycin. Bacterial growth and replication are inhibited by its binding to the bacterial ribosome, which prevents the bacteria from producing new proteins.
- In contrast, Cephalexin, a beta-lactam antibiotic, works by inhibiting an enzyme that forms part of the cell wall of bacterial organisms. It stops the bacteria from forming an outer layer that can resist deformation, which results in the lysis or rupture of the cell wall and ultimately leads to the death of this organism.
By examining the impact of different antibiotic mechanisms on different stages of protein synthesis, it is possible to gain valuable insights into which antibiotics are most effective in eradicating various types of infections. The mechanism of action of cephalexin differs from that of azithromycin, as it primarily targets Gram-positive and some Gram–negative bacteria but is more selective for Gram-1 pathogens.
- Various bacterial infections, such as pneumonia, bronchitis, and other forms of strep throat, as well as skin infections and urinary tract infections, are treated with antibiotics. However, the decision between azithromycin and cephalexin is influenced by the type of infection (such as fever or allergies), the severity of the infection, and patient factors.
- For respiratory infections such as pneumonia, Azithromycin is often the drug of choice due to its ability to persist in lung tissue for a prolonged duration while remaining active against bacteria.
- When treating infections involving skin and soft tissues, Cephalexin may be a more effective treatment option due to its faster absorption into the bloodstream and its ability to penetrate affected areas.
By understanding the distinct mechanisms of action between azithromycin and cephalexin, healthcare providers can make informed decisions about which antibiotic to prescribe for a given infection, ultimately leading to more effective treatment outcomes.
Types of Infections Treated
Both azithromycin and cephalexin are antibiotics designed to treat broad-spectrum bacterial infections. They differ in their specific mechanisms of action and spectrums of activity but share some commonalities when it comes to the types of infections they target.
- Bacterial pneumonia.
- Exacerbations of chronic bronchitis.
- Skin and soft tissue infections (cellulitis).
- Children with otitis media in the middle ear.
- What are UTIs?
Cephalexin, an antibiotic that is sold as a tablet, has been shown to be effective against gram-positive cocci (e.g., Staphylococcus aureus and Streptococcus) and other pyogenes. It is frequently prescribed for skin and soft tissue infections such as cellulitis and abscesses.
- Impetigo (bacterial skin infection)
- Hair shedding inflames the hair follicles.
- Urine infections caused by E. coli.
Despite its broad spectrum of activity, Azithromycin, which is a macrolide antibiotic against different types of bacteria, can still kill gram-negative pathogens like Haemophilus influenzae and Moraxella catarrhalis. Often, it is prescribed for respiratory infections like community-acquired pneumonia and chronic bronchitis.
- Throat infection or perioditis.
- Tonsilelitis.
- Bronchitis.
- pneumonia caused by Mycoplasma pneumoniae and Chlamydophila pneumatosis.
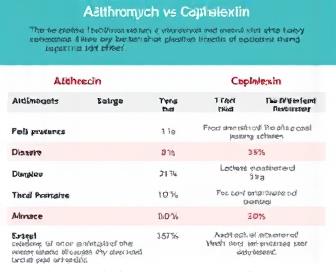
Side Effects Compared
Like all antibiotics, Azithromycin and cephalexin can also cause side effects. Despite the fact that these drugs are generally safe to use as directed, some patients may experience adverse effects from one or both of them. It's essential to weigh the potential benefits of each antibiotic against its possible drawbacks to make an informed decision about which medication is best for your infection.
The degree of side effects can differ significantly based on various factors, including age, overall health status, and the specificity of particular medical conditions. We'll compare azithromycin and cephalexin and discuss some common side effects to help you understand which one is more effective for your health.
Azithromycin Side Effects
- Up to 10% of patients experience nausea and vomiting.
- Abdominal pain or cramping (5-10%)
- Diarrhea (within 6%)
- The range of headaches (4-7%) is a significant problem.
- Allergic reactions, including hives and itching (less than 2%)
- The area where a rash or skin rashes are present (1-3%) is usually not severe.
Cephalexin Side Effects
- Dizziness or lightheadedness (5-10%)
- The range of headaches (4-7%) is a significant problem.
- A potential cause of nausea and vomiting (up to 6%).
- Gastrointestinal problems, including stomach discomfort and diarrhea (3-6%).
- Allergic reactions, including hives and itching (less than 2%)
- It is more likely to have bleeding or bruising (infrequent) as compared to other conditions.
While both azithromycin and cephalexin can cause similar side effects like nausea, vomiting, and diarrhea, some adverse reactions are more common with one medication than the other. Those taking cephalexin tend to experience allergic reactions, and those experiencing abdominal pain (to a certain level) with azithromycin are also slightly more likely.
It's important to keep in mind that these side effects are usually short-term and mild, fading away once the antibiotic treatment is over. Rare instances may result in severe or life-threatening reactions. Consult your doctor immediately if you experience any unusual symptoms while taking either medication, and they may advise you on how to manage them accordingly.
It is important to keep in mind the specific instructions your doctor has given you regarding the amount of medication you should take, the duration of your treatment, and any potential interactions with other drugs. Your infection will be well-controlled, and potential adverse effects will decrease with this step.
Dosage and Administration
The dosage and administration of azithromycin and cephalexin vary slightly between oral and injectable formulations. The dosage of medication that is appropriate for each infection depends on factors like age, weight (penis), type, and severity.
Azithromycin Oral:The recommended dosage for adults with mild to moderate infections is 250-500 mg/day every 2-5 days. In severe or life-threatening cases, higher doses of up to 1-2 grams per day may be prescribed by a healthcare professional.
Cephalexin Oral:In adults, the recommended oral dosage for cephalexin is between 250 and 1000 mg every 6-8 hours for mild to moderate infections. Maximum per day, 4 grammes or so. More severe infections may require longer treatment courses or higher doses under medical supervision.
Azithromycin Injectable:Typically, patients in the hospital who require IV treatment due to severe infections are given azithromycin as an infusion of 500-1000 mg every 24 hours for that period. The recommended period of survival is determined by the type and severity of the infection, which can range from 3 to 14 days.
Cephalexin Injectable:The usual dosage of cephalexin is 500-1500 mg every 6-8 hours, and it is given intravenously for severe infections that require hospitalization. It is recommended that the total dose be no more than 4 grams/day and that each treatment course usually lasts 7-10 days or more, depending on need.
These antibiotics should be taken with extreme care by your doctor. Medications may not be administered correctly or prescribed at times, which can result in inadequate treatment effectiveness and potential antibiotic resistance, as well as serious side effects.
Choosing the Right Treatment Option
When dealing with an infection, it is crucial to determine which antibiotic is most effective and safe to use in order to minimize the risk of side effects. Azithromycin and Cephalexin are two of the most frequently prescribed antibiotics, but they have distinct properties that make one more effective for specific infections than the other.
Consider the nature of your infection. Azithromycin's broad-spectrum action against different bacterial strains, such as Mycoplasma and Chlamydophila, is frequently necessary for the treatment of respiratory tract infections like pneumonia or bronchitis. On the other hand, Cephalexin's beta-lactam structure may be more effective in treating skin and soft tissue infections that involve cellulitis or abscesses, as it specifically targets gram-positive bacteria.
Moreover, assess the extent of your infection. The longer half-life of Azithromycin and its ability to concentrate in tissues make it a preferred choice for serious or life-threatening conditions, where it can provide antibiotic activity that is sustained. Cephalexin is typically used for less severe infections that do not require extended exposure.
Depending on the individual's age, weight, and medical history (such as family history or older siblings), which antibiotic is best for them all depends on what. Children under 16 years old may benefit from Azithromycin's pediatric formulations and tolerability profile. At the same time, individuals with kidney or liver impairment may need to modify their Cephalexin dosage as the drug may accumulate.
Finally, take into account your individual preferences and circumstances (e.g., allergies, prior exposure to certain antibiotics, etc.). Discussing these factors with your physician can help you in determining which antibiotic is most effective for you.
- Broad-spectrum activity makes Azithromycin suitable for respiratory infections like pneumonia or bronchitis.
- The use of Cephalexin, which has a beta-lactam structure and targets the majority of bacteria in your system, especially gram-positive bacteria, makes it an effective treatment for skin and soft tissue infections.
- Due to its longer half-life and higher tissue concentration, Azithromycin is a more effective treatment option for severe or life-threatening conditions.
- Azithromycin is a safe and effective drug for children under 16 years of age, as it can be administered in pediatric doses.
- Cephalexin dosage adjustments may be necessary in patients with kidney or liver impairment.
- Identify and discuss personal circumstances, allergies, and sensitivities when choosing an antibiotic.
With the knowledge of these factors and an in-depth discussion with your doctor, you can determine which antibiotic is most effective and safe to use for your infection, resulting in a successful recovery process.
We recommend you read it
There are several pages on our website that you should read if you have been given Cephalexin.
- Why does CephalexIN smell bad?
- How should Cephalexin be used?
- What are the side effects of Cephalexin?













