ADS:
Bumex to Lasix Conversion Guide - Understanding Equivalent Doses and Potential Risks
In cases where fluid buildup is a concern for the body, physicians often turn to loop diuretics like Bumex and Lasix. Although the drugs have a common function, their chemical compositions and potential side effects vary. The conversion of patients from Bumex to Lasix nécessites careful consideration of similar doses and potential risks.
The precise understanding of this conversion is essential for achieving optimal patient outcomes. As an example, a study published in the American Journal of Kidney Diseases found that it is important to know what dose is right when you switch patients from Bumex to Lasix. The study revealed that erroneous dosage can result in inadequate diuresis, electrolyte imbalances (and even an increased risk of acute kidney injury).
A healthy strategy involves educating patients about the advantages and disadvantages of each medication, as well as closely monitoring their reaction during the transition phase. To ensure a seamless transition from one patient to another, healthcare providers can use bumex (i.e., bummer's scale) versus lasix comparison charts and conversion calculators as resources.
To ensure patients are treated as well as they were before the Bumex-to-Lasix conversion, healthcare professionals should carefully consider the risks associated with such a conversion. The following is a protocol for key considerations to help you successfully re-dispatch your patients from Bumex to Lasix so that you can continue to provide excellent care and improve overall patient satisfaction.
Bumex To Lasix Conversion Guidelines And Protocol
When changing the treatment from Bumethanide (Bumex) to Lasix, several factors, such as the patient's underlying health condition and their renal function, as well as their reaction to both diuretics, must be considered. To ensure a seamless transition from Bumex to Lasix while still receiving the best therapeutic outcomes, this protocol provides.
Conversion should be evaluated before beginning with the patient's current regimen (dosing, frequency, and concomitant medications that may affect the efficacy or safety of diuretics). Acquire a comprehensive medical report, with emphasis on factors such as health problems (common ailments), allergies, and previous interactions with loop diuretics. Monitoring kidney function by analyzing laboratory tests, with a focus on serum electrolytes (sodium, potassium) and creatinine levels.
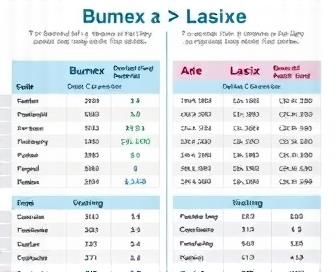
Calculate the equivalent furosemide dosage for a patient receiving bumetanide at present. It is common for people to convert their Bumex doses into the following as:
- 0.5 mg Bumex = 40 mg Lasix.
- 1 mg Bumex = 80 mg Lasix.
- 2 mg Bumex = 160 mg Lasix.
- 3-4 mg Bumex = 240-320 mg Lasix (dose increment in 40 mg increments)
To ensure compliance with the recommended dose-to-volume ratio, patients who are currently receiving bumetanide should adjust their conversion rate accordingly. The midpoint of a patient taking 2.5 mg Bumex would be 160-240 mg, and the medication Lasix would replace the excess fluid at around 200 mg.
Use the following steps to switch from Bumex to Lasix:
- Take the equivalent dose of furosemide and bumetanide together and then give it at that rate to your body.
- To ensure a specific diuretic effect, it is important to closely monitor the patient's response and adjust the dosage of Lasix accordingly.
- In case of reduced responsiveness, it is advisable to increase the dosage of Lasix gradually from 20-40 mg every 2-3 days until an appropriate response is attained.
- When administering IV fluids and re-evaluating electrolyte levels in patients with severe dehydration or electrolytic imbalances after conversion, it is important to consider the effects of any changes in electrolysis before making dosage adjustments.
Take into account the patient's clinical status, serum electrolytes, and renal function on a regular basis during the transition period. Please prefer to modify the amount of Lasix you administer according to the patient's treatment if required. Properly formulated guidelines and protocol steps can facilitate the conversion from bumetanide to furosemide while minimizing potential side effects and improving therapeutic outcomes for patients with fluid overload or edema.
Indications And Mechanism Of Action Comparison
Loop diuretics Bumex (methoxyflurane) and Lasix (furosemide), among other heart disease drugs, are used. Despite their differences in mechanism of action, efficacy, and indications for urine production, both medications have been found to increase urine output.
By inhibiting the sodium-potassium-chloride cotransporter in the thick ascending limb of the loop of Henle, Bumex and Lasix are loop diuretics that lead to increased excretion of water and electrolytes from the descending lobe. But they differ in one thing, their pharmacology:.
- Unlike Lasix, which takes up to 1-2 hours to activate in the body at first, Bumex has a slower onset of effects.
- Diarrhea can be induced more rapidly with Lasix, within 30 minutes to 1 hour after administration.
| Medication | Indications |
|---|---|
| Bumex (Methoxyflurane) | Severe hypertension, pulmonary edema, heart failure, and ascites. |
| Lasix (Furosemide) | Hypertension, congestive heart failure, acute renal insufficiency, edematous states, nephrotic syndrome, and idiopathic edema. |
Despite both being available, Lasix is the preferred medication for managing hypertension because of its faster action. However, Bumex may be more suitable for severe pulmonary embolism or ascites because of its prolonged and slower diuretic impact.
The decision to use Bumex versus Lasix is determined by the clinical situation and individual patients. The selection of a loop diuretic for use in patients requires healthcare providers to take into account these variations.
Conversion Criteria And Patient Selection Factors
Bumex can be converted to Lasix with some degree of caution, but there are several important factors that must be considered, such as patient selection criteria and specific clinical situations where conversion is most effective. These loop diuretics are based on individual patient characteristics, disease states, and treatment goals.
- Patient characteristics such as age, weight, and other factors such as the patient's renal function, electrolyte status, comorbidities (such as gout [see description]), and what medications they are taking make up the decision to switch from Bumex to Lasix.
- Disease states: Special diuretic treatment may be necessary for certain conditions, such as heart failure, cirrhosis, or nephrotic syndrome. Bumex may be more effective than Lasix in patients with volume overload caused by liver disease, as it has a shorter duration of action.
- The choice between these loop diuretics and other treatments is influenced by the desired level of diuresis and the need for potassium-sparing effects. If patients need more aggressive diuresis, the stronger natriuretic effect of Lasix may be preferable.
Before converting from Bumex to Lasix, it is important to consider these factors and weigh the benefits against potential risks. The conversion process necessitates a thorough evaluation of patient requirements and careful testing for appropriateness.
- Start with a low dose: When switching from Bumex to Lasix, begin at a lower dose (e.g., 20 mg) and gradually increase as needed to avoid excessive diuresis or electrolyte disturbances.
- Keep an eye on side effects: closely monitor patients for signs of dehydration, electrolyte imbalances, or other negative consequences that may occur during the conversion process.
Clinical professionals should carefully consider these factors and follow well-established conversion guidelines to ensure that patients are treated with the best outcomes from their initial diuretic Bumex to Lasix.
Stepwise Bumex To Lasix Titration Protocols
Step by step, to ensure patients have optimal fluid management and minimize potential adverse effects, the transition from Bumex to Lasix requires careful consideration of each patient's body. This section details the steps required to titrate Bumex and Lasix.
Protocol 1: Mild to Moderate Edema.
- To achieve a diuretic effect similar to that of bumetanide (Bumex), administer 10-20 mg of furosemide (Lasix) PO/IV every 6-8 hours, starting with the lowest dose.
- In case the edema improves but the patient still needs more diuresis, increasing the dose of Lasix by 10–20 mg every 3-4 days is recommended until the response is at an optimal level.
- Examine for potential over-diuresis or electrolyte imbalances and modify the furosemide dosage accordingly.
Protocol 2: Severe Edema or Heart Failure.
- In patients with severe edema or heart failure, it is recommended to start Lasix at a higher dose of 40-80 mg PO/IV every 6 hours to quickly reduce fluid overload and improve hemodynamics.
- If necessary, increase the dosage of Lasix by 20-40 mg every 3 or 4 days until an optimal response is achieved, then taper it off as needed for maintenance therapy.
- Take care not to over-diureze (especially in patients with impaired renal function or those with existing electrolyte imbalances) and adjust the furosemide dosage accordingly.
Protocol 3: Bumex to Lasix Conversion in Renal Impairment.
- For individuals suffering from significant renal impairment (CrCl <30 mL/min), patients may receive Lasix at a dose of 10-20 mg PO/IV every 12 hours, with careful consideration for any signs of over-diuresis or electrolyte imbalances.
- The Lasix should be given in 5-10 mg increments every 3-4 days if the patient's fluid condition improves, with the aim of monitoring renal function and electrolytes to monitor these changes.
- Adjust the furosemide dosage to achieve the most effective diuretic effect with minimal side effects.
Specifications.
- Keep a watchful eye on patients during the titration procedure to detect indications of excessive diuretic activity, electrolyte imbalances (specifically potassium and magnesium), as well as worsening renal function.
- Observe the potential interactions between bumetanide and furosemida, as well as other medications that may be prescribed at appropriate intervals to minimize adverse effects.
- It is important to ensure that patients are hydrated before switching from bumetanide to Lasix.
The conclusion.
By following a well-planned stepwise titration protocol, patients can be converted from the high-risk drug Bumex to the low-level medication Lasix, which can help reduce the risk of side effects and improve fluid retention. Healthcare professionals can tailor a plan of action to suit the individual needs of patients, taking into account factors such as disease severity and renal function, to ensure optimum success in the transition.
Monitoring Parameters For Safe Transition
The aim of the voluntary change from Bumex to Lasix is to make sure that patients do not experience any unfavorable effects or worsen in their clinical situation. achieving this by closely monitoring parameters.
- To determine if the patient is dehydrated or overhydrated, it is important to conduct a physical exam and assess their fluid status through blood tests, vital signs (BP, HR), and laboratory analysis (BUN/Cr ratio).
- Prevent diuresis: Bumex can induce more severe episodes than Lasix. Monitoring urine output and adjusting fluid replacement accordingly helps prevent excessive volume depletion.
- Ensure that electrolyte balance is maintained by closely monitoring serum electrolytic components, including potassium, sodium, and magnesium; the use of Lasix can lead to hypokalemia. Replenish deficient electrolytes promptly if necessary.
- The biochemical parameters of renal function are determined by monitoring blood urea nitrogen (BUN), creatinine, and uric acid levels on a yearly basis to identify potential signs of nephrotoxicity or exacerbation of existing kidney disease.
- Alter the dosage of Lasix as needed: Based on biochemical parameters, adjust the dose accordingly to achieve the best diuretic effect possible without causing any adverse effects.
Safe transition is also dependent on patient education and close physician supervision. Provide patients with information about potential side effects, prompting them to report any issues promptly, and continuously review the patient's response to therapy throughout the transition period.
Common Complications And Management Strategies
It is important for healthcare providers to be cognizant of the potential complications that may occur during the bumex to lasix conversion process, in addition to following all necessary guidelines and protocols. Electrolyte imbalances, particularly hypokalemia, can cause cardiac arrhythmias or muscle weakness. The elimination of chloride ions from the body is a common cause of metabolic alkalosis. Negative symptoms like nausea, vomiting, and dizziness may occur due to inadequate conversion rates or sudden changes in diuretic treatment.
It is important to closely monitor patients' electrolyte levels during bumex-to-lasix conversions. To achieve this objective, it is necessary to conduct regular tests on serum potassium, sodium (calcium iodide), chloride, bicarbonate, and magnesium. Depending on the patient's needs, patients may be given potassium supplements, or the rate of conversion can be adjusted as part of the corrective action.
Metabolism associated with metabolic alkalosis can be regulated by various treatments, such as acetazolamide (an antibiotic that causes elevated urinary bicarbonate excretion) or other agents. Sodium chloride infusions may be required to restore equilibrium in severe cases. It is important for healthcare providers to collaborate with patients and their families during this transition period to ensure they are aware of the importance that there may be when it comes to following a consistent medication regimen and dietary changes.
In the event of a potential problem, it is crucial to keep an eye on patient status and modify treatment plans accordingly. Altering the conversion speed or adding other drugs to stabilize electrolyte levels is one option. Keeping this in mind, healthcare providers must be proactive and work with patients to minimize the risk of side effects that may occur as a result of bumex-to-lasix conversions; therefore, they can improve the outcome of their treatment through these efforts.
At the end of the day, a multidisciplinary approach is necessary to address the issues associated with bumex to lasix conversion. This entails having an open dialogue with caregivers, regular observation, and prompt intervention in the event of complications. Through this process, healthcare providers can teach patients about how to maintain fluid balance and high electrolyte levels in a manner that is both safe and healthy, which will ultimately improve overall health.
Evaluation Of Conversion Outcomes And Follow-Up Plans
To achieve a bumex to lasix conversion, meticulous planning, precise dosing, and close patient monitoring are necessary. After transitioning patients from bumex to lasix, healthcare providers must evaluate the outcomes of this process to ensure that the chosen therapy is effective in managing their edema and hypertension. The subsequent part covers the essential elements of assessing conversion results and devising follow-up plans to ensure patient care is maintained at an exceptional standard.
- Examining Conversion Outcomes.
- This study examines the impact of lasix on patient health by examining changes in edema, blood pressure, and electrolyte levels.
- Observe any potential side effects or adverse reactions to the medication, such as increased urine output, dehydration (due to low blood pressure), or potassium levels.
- To ensure a correct substitution ratio, compare bumex dosing before and after conversion to lasix after each dose change.
The maintenance of therapeutic effectiveness and minimizing adverse effects are essential for patients who require ongoing management with lasix, and regular follow-up appointments are necessary. Healthcare providers are advised to:
- Assess the patient's well-being by examining their progress and altering medication regimens accordingly to achieve optimal control of swelling and blood pressure.
- Monitor potassium levels closely to ensure no potential imbalances are present.
- Ensure that patients are aware of the risks associated with using their prescribed lasix regimen and seek medical attention if they experience any side effects, such as urine ingestion or loss of fluid retention.
- Seeking professional advice on managing complex edema or hypertension is suggested, and it may be best to seek the help of a specialist such as a nephrologists.
When Lasix is not able to respond adequately or causes severe side effects, it may need to be modified or stopped in some cases. In such cases, healthcare practitioners may consider other diuretic treatments or non-pharmacological measures such as dietary modifications and fluid control strategies. It is important for patients to understand that modifying their treatment plan is often necessary in order to achieve the best possible outcomes.
If you want to learn more about Lasix dosage instructions and conversion methods, including the potential for crushing Lassie, check out this informative article.
We recommend you read it
To learn more about the impact of Lasix on BNP levels, check out this article.
- In this article, you'll learn about the connection between furosemide (Lasix) and Brain Natriuretic Peptide (BNP), a hormone that helps regulate blood pressure.
See our article for more information on why you might not feel comfortable while taking Lasix due to swelling in your feet, which can be found here.
- It details possible causes of this side effect and how to manage it.
Torsemide is sometimes required in place of Lasix. Our article at this link provides additional information on when to switch.
- In this article, you'll learn about the distinctions between these two diuretics and their potential uses in different contexts to achieve optimal health outcomes.













