ADS:
Fibroid Treatment Options with Tamoxifen
Urokine: Doctors often use multiple treatment options to treat uterine fibroids and improve patient health. A potential alternative to tamoxifen for treating uterine fibroids, which is a traditional method of breast cancer treatment, has gained more attention in recent times. Before diving into this novel technique, it's crucial to comprehend how tamoxifen and fibroids might interact at a deeper level.
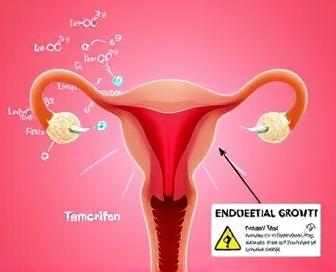
Fibroids, which are benign growths inside the uterus, are common and often cause women to experience heavy menstrual bleeding, pelvic pain, or other discomfort symptoms. Fibomas are generally benign, but there is a possibility of developing cancer under specific circumstances. Uterine fibroids are best treated by carefully considering the impact this has on endometrial growth and, therefore, cancer risk.
The addition of tamoxifen to traditional fibroid treatments - such as hormone therapy, uterine artery embolization, or even surgery - may offer certain benefits for select patient populations. Tylenosides may be targeted by tamoxifen to decrease the growth of fibroid tissue and alleviate symptoms of severe bleeding caused by estrogen-induced hemorrhaging. Nonetheless, it's important to weigh these potential benefits against the fact that tamoxifen can also heighten the likelihood of developing endometrial cancer in women who use it for an extended duration.
Given the increasing complexity of how fibroids, tamoxifen, and endometrial growth interact, it is important for physicians to consider patient factors such as a woman's antenatal history (if any), hormone levels, genes, or other factors when suggesting treatment courses that may include these medications. Their approach involves minimizing risks and optimizing therapeutic outcomes for their patients.
We'll go over the scientific basis for tamoxifen as a cure, provide details on its safety and effectiveness in treating uterine fibroids, analyze current data to determine whether it is safe or effective for these indications, and outline some important factors that healthcare professionals and patients should be aware of when dealing with these complex issues. Our understanding of the connections between fibroids, tamoxifen, and endometrial health can aid in developing more effective patient-centered strategies for managing this prevalent gynecological disorder.
Fibroids & Tamoxifen: Understanding the Risks
Breast cancer is typically treated or prevented from recurring with the help of Tamoxifen, an estrogen receptor modulating medication. Despite its significant advantages in reducing the likelihood of developing breast tumors related to estrogen receptor positive genes, tamoxifen may result in unwanted side effects, particularly in individuals with fibrous tissue.
Non-cancerous bumps inside the uterus, known as fibroids (ileous masses), can cause symptoms such as intense bleeding and pain in the pelvis or pressure on the surrounding organs. Tymofen may be required when a woman has fibroids, and the hormone can cause endometrial thickening or hyperplasia.
- The American College of Obstetricians and Gynecologists (ACOG) recommends that women with uterine fibroids who are considering tamoxifen therapy undergo a thorough evaluation, including an endometrial biopsy or ultrasound, to assess their risk for endometrial hyperplasia or cancer.
- If a woman has had abnormal pap smears, if her doctor has previously diagnosed her with AP-CB (intermittent methamphetamine), or other irregularities in the testicles or upper abdomen, she should take extra care to closely monitor her endometrial health under expert guidance when taking tamoxifen.
- Uterine sarcoma, an aggressive cancer that can develop in fibroids or other parts of the uterus, is a rare but potentially life-threatening condition that may arise from tamoxifen use. Despite being low, this risk highlights the need for regular screening and monitoring to detect abnormal cell proliferation.
- If a woman is taking tamoxifen and experiencing vaginal bleeding, pelvic pain, or other symptoms that may indicate endometrial thickening or hyperplasia, she should immediately notify her doctor.
Tamoxifen therapy should not be sidestepped by women who are considering it, as they should openly communicate with their healthcare providers about the potential risks and benefits. Women should be monitored regularly and carefully consider these factors before choosing their treatment options, which can help them avoid the risks associated with combining tamoxifen and fibroids.
What are Fibroids?
The smooth muscle of the uterus is where benign tumors known as fibroblastas are commonly found, also known in some cases as "uterine leiomyomas." Women of all ages can be affected by these changes, which can vary from small to large in size but are typically seen during the age range of 30-50.
These growths can develop either inside or outside the uterus and may cause periods that are heavy, frequent pelvic pain, urine incongestion, or constipation. Infertility problems may arise in women with fibrosis.
Growth of the fibromy gland is dependent on several factors, including genetics as well as hormones and the environment. fibroid) development because the receding levels of estrogen and progesterone (which both are important hormones in hormonal regulation) lead to the shrinking of fibroids after menopause.
- There are three main types of fibroids: intramural (growing within the uterine wall), subserosal (growing under the outer lining of the uterus), and pedunculated (hanging from a stalk).
- One or more fibroids is common, and their size can differ significantly.
Despite their non-cancer characteristics, fibroids can still lead to uterine cancer in certain cases. The reason why women with fibroids should undergo regular check-ups and screening tests to detect any complications or changes over time is important.
Tamoxifen Use and Cancer Risk
The use of Tamoxifen, an estrogen receptor modulator (SERM), is primarily directed towards women at high risk for breast cancer, especially those with genetic mutations or family history. While it has been proven to have positive effects on breast health, there are concerns about its possible impact on endometrial development and the risk of cancer.
- Endometrial polyps and hypertlasia, which can develop into cancer if left untreated, are more common among women who use tamoxifen over an extended period, according to research.
- While the precise causes of this increased risk remain uncertain, it is hypothesized that tamoxifen's anti-estrogen impact on the breast may have an estrogenic effect on blood vessels in the endometrium, which could lead to cell growth and proliferation.
A consistent and strong correlation has been found between extended use of tamoxifen (often denoted as 2 years) and an increased risk of endometrial cancer. The risk of developing endometrial cancer was found to be approximately twice as high in women who took tamoxifen for more than 24 months than those who received placebo or no treatment, according to a meta-analysis of 14 studies conducted in 2013.
- The relative risks of endometrial cancer in patients who take tamoxifen have been found to increase in several large clinical trials, with estimates ranging from about 1.5% at time of administration to as early as 2 years after completion, and this is subject to variations in risk per study and duration of treatment.
The findings suggest that tamoxifen treatment should include close monitoring for signs and symptoms of endometrial disease. If a woman experiences any unusual bleeding or discharge in her vagina, it is recommended that she notify her doctor immediately and may undergo periodic ultrasound tests for abnormal bleeding during or outside of the vagina.
Endometrial Growth Implications
The growth of endometrial tissue can be influenced by benign fibroids located in the uterine wall. Endometrial growth can be stimulated by Tamoxifen, a hormone therapy medication commonly used for breast cancer treatment.
The potential for tamoxifen to increase endometrial growth may be particularly concerning in women with fibroids, as these growths can lead to altered uterine anatomy and potentially disrupt hormonal balance. Optimal growth and endometrial cancer risk may increase due to the potential stimulatory effects of this combination.
Excessive cell proliferation in the endometrium, also known as endochlorine (endostatin), is believed to be a common cause of endogenous disease, with increased rates of use of tamoxifen. This hyperplasia may be more prominent in women with fibroids, and their altered tissue dynamics could increase their susceptibility to endometrial cancer at some point.
While some research suggests that tamoxifen's effects on endometrial growth may be less significant than previously thought, particularly when compared to other estrogen-based therapies, it remains essential for women with fibroids to have open and informed discussions with their healthcare providers regarding potential risks. Care for this population requires thorough monitoring of endometrial health and regular screening for abnormalities.
Research on the Connection
The possible association between fibroids and tamoxifen has been investigated, with particular attention given to its potential to hinder endometrial development and increase the likelihood of cancer in women with uterine leiomemes. Scholars aim to comprehend how these interactions are driven.
- The estrogen receptor modulator tamoxifen is commonly used for breast cancer treatment and prevention. Its anti-estrogen properties can also affect the uterus, potentially influencing fibroid growth and endometrial cell behavior.
- In certain cases, researchers have found that tamoxifen may promote the growth of fibroid cells, which can result in increased mass in the uterus and potential complications such as heavy menstrual bleeding or untimely termination of pregnancy.
Other investigations found that the effects of tamoxifen on fibroids may depend on factors including size of the fibroid (the normal diameter of an endocardium), subtype of that particular vascular fiber, and patient's age. Smaller fibroids may be more responsive to tamoxifen than bigger ones.
- A systematic review conducted 11 studies on the effectiveness of tamoxifen for treating fibroids in women. Some studies suggested a connection between tamoxifen usage and endometrial hyperplasia or cancer, but this was not the case.
The intricate connection between fibroids, tamoxifen, and endometrial health necessitates additional research. Specifically, the investigation should include factors like patient characteristics, subtypes of the fibroid system, and possible interactions with other agents such as medications or hormones.
- The long-term effects of tamoxifen therapy on women with fibroids should be taken into account in future research, as they can offer more precise guidance for clinical management strategies.
Potential Complications & Prevention
Fibroblasts and tamoxifen can cause complications that are particularly concerning in women with endometrial growth and cancer. These drugs can be very successful at treating symptoms and reducing the risk of developing uterine cancer, but they have some drawbacks which must also be considered in relation to one's own situation.
The growth of the follicle may accelerate during tamoxifen treatment due to hormonal changes, which could lead to increased pain, bleeding, and other complications. Moreover, prolonged exposure to tamoxifen can increase the risk of endometrial cancer, particularly for those with pre-existing fibroids or a history of estrogen-receptor positive breast cancers.
A healthcare provider must closely monitor patients during treatment to minimize risks. To monitor hormone levels and detect early signs of endometrial thickening or abnormal cell growth, pelvic exams, ultrasound assessments, and blood tests are frequently used as regular check-ups. In some cases, fibroids may need to be surgically removed prior to tamoxifen initiation or during the course of therapy if they show signs of rapid progression.
Proper dosages and treatment plans as directed by a healthcare provider are essential in preventing complications. The recommended steps for women taking tamoxifen are to abstain from hormonal birth control, avoid smoking, and maintain a healthy diet consisting mostly of fruits, vegetables (especially green), whole grains (including dark or black meat), and exercise regularly while working out.
Open communication with one's healthcare team is essential during the treatment process. The combination of staying informed about potential complications and working together to develop personalized prevention strategies can aid in managing fibroids and tamoxifen therapy, as well as reduce the risk of endometrial growth and cancer.
Fibroid Management Strategies
In order to effectively manage fibroids, one must take into consideration the individual characteristics of each symptom setter as well as the size and location of the growths in the developing area, as adults age with them, overall health conditions (if present), and personal preferences. The process often involves exploring various treatment options to determine the most appropriate option for women.
Menstrual pain and other symptoms associated with fibroids can be greatly reduced by medication. Hormonal therapies, such as birth control pills or gonadotropin-releasing hormone (GnRH) agonists, may help reduce heavy bleeding and alleviate cramping by suppressing uterine growth and contractions. Ibuprofen and other NSAIDs are effective in curing pain.
Women with larger or more problematic fibroids frequently undergo surgical procedures. Myomectomy, a procedure to remove the fibroid while leaving the uterus intact, offers potential relief from symptoms and may improve fertility in some cases. Using a hysteroscope and specialized instruments, sex is done to remove fibroids from the uterine cavity through hypnosis, which is another option for minimally invasive surgery.
Urine embolization (UAE) may be suggested in certain cases. This is a minimally invasive procedure whereby small particles or substances are injected into the blood vessels that supply nutrients to the affected fibroid, which in turn causes its growth to slow down over time.
Women who have undergone conservative treatments or have a larger uterus may require a hysterectomy to be removed. The majority of times, this surgical procedure is successful in reducing symptoms, but it involves the permanent removal of the uterus and potential disruptions to future fertility.
| Treatment Option | Potential Benefits | Potential Risks/Side Effects |
|---|---|---|
| Hormonal Therapies (e.g., birth control pills, GnRH agonists) | Reduced heavy bleeding and pain relief | Changes in menstrual pattern or cessation, potential hot flashes, mood swings |
| Myomectomy | Potential symptom relief, improved fertility (in some cases) | Risk of complications during surgery, possible recurrence of fibroids |
| Hysteroscopic Resection | Minimally invasive, potential for same-day discharge | Moderate-to-severe cramping, risk of infection or uterine perforation |
| Uterine Artery Embolization (UAE) | Potential symptom relief without surgery | Risk of complications during procedure, possible recurrence of fibroids |
| Hysterectomy (uterine removal) | Permanent symptom relief, potential improvement in menopausal symptoms for some women | Permanent loss of fertility, potential risks associated with major surgery |
Talking to a doctor about your condition and treatment options is crucial. You have the option to evaluate the benefits and drawbacks of each method, and your doctor can assist you in determining the most effective way to treat your fibroids. To illustrate, Lasix skin rash pictures could be a potential drawback of hormonal treatments.
Fibroblast management necessitates a multifaceted approach that considers all treatment options and individual circumstances. By understanding the potential benefits and risks of each strategy, women can make informed decisions about their care and work with healthcare providers to achieve optimal symptom relief and quality of life.
We recommend you read it
Here are the resources we recommend for understanding the mechanism of action, effects on male breast development, and common side effects such as leg cramps, along with additional information: Tamoxifen dosage details.













