ADS:
Tamoxifen Necessity in DCIS Treatment Debunked
Recently, there has been a growing controversy surrounding the use of injectable tamoxifen for treating ductal carcinoma in situ (DCIS), characterized by non-invasive breast cancer cases where abnormal cells are located only inside the milk duct. As new research comes to light on the controversial topic, healthcare professionals are questioning whether tamoxifen actually benefits DCIS patients more than it risks.
To fully comprehend the intricacies of tamoxifen's function in DCIS treatment, one must consult current literature. The focus of this article is on the importance of tamoxifen in treating DCIS, with particular attention to its ability to lower recurrence rates and evaluate its impact on quality of life and long-term side effects.
Some research indicates that tamoxifen has the potential to prevent repeat infections in high-risk patients, but its risks of endometrial cancer and blood clots make its benefits unestimable. Many patients are left inconsolable as the controversy has erupted into heated discussions within medicine, leading to questions about their treatment options.
Our ongoing dialogue will also address non-tamoxifen options for DCIS management, including radiation therapy and close monitoring. The link between Lasix and sulfa, as noted in this research, may also aid in reducing the risk of DCIS recurrence by including a healthy diet consisting mostly of fruits and vegetables.
We will explore the current evidence regarding tamoxifen's role in managing DCIS and highlight both supporting and opposing research in this article. Our goal is to provide patients with a balanced perspective on their healthcare needs, which they can use as guiding questions.
Tamoxifen Necessity in DCIS Treatment - A Comprehensive Overview
Non-invasive forms of breast cancer, known as ductal carcinoma in situ (DCIS), involve the confinement of abnormal cells within the aortic glands. Although not invasive, untreated DCIS can develop into breast cancer invasion. Thus, the focus should be on developing treatment plans that minimize the risk of a repeat episode and maximize patient outcomes.
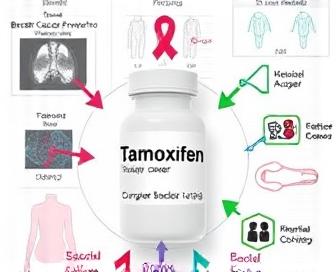
Tamoxifen is among the primary drugs utilized for DCIS. Tamoxifen selectively represses estrogen receptors by binding to them, and this mechanism of action prevents cancerous cells from growing or multiplying. Studies have extensively examined the impact of Tamoxifen on the risk of recurrent DCIS and invasive breast cancer.
The efficacy of tamoxifen in DCIS treatment is supported by numerous clinical trials. Adjuvant tamoxifen was found to have a significantly lower risk of ipsilateral (in the same breast) recurrence compared to observation alone, according to a landmark study published in The Lancet in 2013 that showed how adjuvant therapy could reduce the risk.
The risks and side effects of tamoxifen are not universally accepted. In high-risk patients, the adverse effects include hot flashes and dryness of the vagina as well as being more likely to cause blood clots or stroke. When evaluating the potential effects of certain types of tamoxifen on individuals with DCIS, healthcare providers must carefully weigh the pros and cons.
| Study | Patient Population | Treatment Arms | Results |
|---|---|---|---|
| NSABP B-24 (2013) | DCIS patients with estrogen receptor-positive tumors | Adjuvant tamoxifen vs. observation | Tamoxifen significantly reduced ipsilateral recurrence risk |
| IBCSG-1 (2014) | DCIS patients with high-risk features | Adjuvant tamoxifen vs. observation | Tamoxifen improved recurrence-free survival and overall survival |
| AZTEC trial (2018) | DCIS patients with low- to intermediate-risk features | Adjuvant tamoxifen vs. observation | No significant difference in recurrence rates between arms, but tamoxifen reduced contralateral breast cancer risk |
The use of Tamoxifen in DCIS is essential because it lowers the risk of recurrence and invasive disease. It's not without risks, but if you are careful in selecting and monitoring your patients, the risk is very low because it will minimize adverse effects at the expense of all the benefits.
Understanding DCIS and Its Implications
A type of breast cancer that affects the milk duct cells in situ is known as ductal carcinoma in situ (DCIS). Currently, the cancerous cells have not infected surrounding tissues or any other areas of the body.
An early stage breast cancer, DCIS is frequently presented with no apparent symptoms. Nevertheless, certain females may encounter discharge from their nipples, a swelling in the breasts, or changes in facial structure or volume.
- The formation of small calcium deposits during the proliferation of DCIS cells can be observed on mammography.
DCIS is a type of imaging test that typically includes mammograms and occasionally ultrasounds for diagnosis. Cells are identified through a biopsy procedure.
- Patients who undergo DCIS treatment usually receive a lumpectomy or mastectomy, followed by radiation exposure.
- Hormonal therapy, including tamoxifen, may also be prescribed for some women with DCIS to reduce the risk of recurrence and new primary cancers in the opposite breast.
DCIS-compliant women are more prone to breast cancer invasion. The best course of treatment for them should be based on factors such as tumor size, grade, and hormone receptor status; they must also consult with their doctor.
Knowledge of DCIS and its implications empowers women to take more effective action against breast cancer through proactive management.
The Role of Tamoxifen in Preventing Recurrence
Tamoxifen is a significant estrogen receptor modulator that helps prevent breast cancer, especially in women with ductal carcinoma in situ (DCIS). Detailed research has been conducted to ascertain the effectiveness of this treatment in reducing the likelihood that the illness will occur again after initial therapy. Researchers have found that tamoxifen significantly decreases the likelihood of tumor reappearance and distant metastases.
Evidence suggests that there is a significant decrease in local and systemic recurrences when patients use tamoxifen after DCIS diagnosis, as indicated by consistent research. The Journal of Clinical Oncology published a meta-analysis that revealed an 81% relative risk reduction for ipsilateral breast tumor recurrence (IBTR) was observed with treatment, while the study did not show any significant difference between tamoxifen and placebo.
- In addition, tamoxifen works by inhibiting the binding of estrogen to the estrogen receptors on tumor cells, which in turn slows the growth and proliferation of cancer cells. This prevents estrogen-driven cancer progression and is believed to help the drug prevent recurrence after DCIS treatment.
Some women may not respond to tamoxifen due to their unique characteristics or biomarker profiles. According to the American Society of Clinical Oncology (ASCO) guidelines, individuals with a low oncotype score (OS) - which indicates that minimal genetic activity is responsible for cancer development – may not respond well to adjuvant hormonal therapy such as tamoxifen following DCIS.
There is no consensus on whether tamoxifen can prevent women with low OS scores from experiencing recurrences, although studies have been conducted. The NSABP B-37 study found that there was no statistically significant difference between the IBTR rates of women receiving tamoxifen and placebo, regardless of whether their low or high OS scores were. On the other hand, a different study published in Cancer Research found that tamoxifen treatment resulted in lower recurrence rates for patients with low OS scores than those receiving placebo.
Thus clinicians must carefully consider the patient's individual characteristics, such as their age and other characteristics (such as tumor type or features), menopausal status, and general health, in determining whether they are benefiting from or not using tamoxifen. By taking into account these differences, oncologists can determine if there is a need for tamoxifen to prevent the disease in women with DCIS from reappearing.
Examine the effects of a low oncotype score on tamoxifen usage.
Balancing Benefits and Risks for Patients
It is important to weigh the pros and cons of including tamoxifen in DCIS treatment. Although tamoxifen has been shown to lower the risk of invasive breast cancer recurrence by up to 50%, its use is not without issues.
Some patients, particularly those with a strong family history or genetic mutations at high risk, may find that the protective effects outweigh the individualized risks. Yet, for some, these possible disadvantages might be enormous and have a significant impact on quality of life as well as treatment acceptance.
- Tamoxifen: Riddles:.
The primary hazards of using tamoxifen are:
- Venous thromboembolism (VTE): increased risk of blood clots, particularly in older patients and those with a history of VTE or heart disease.
- Tumor growth associated with tamoxifen increases the likelihood of endometrial cancer and potentially incurable cancer.
- Cataracts and visual issues: patients who use the device for an extended period may develop cataracts, which can lead to blurred vision or other eye movements.
- Some women experience distressing symptoms such as hot flashes and dryness in their vaginas.
It is essential to provide patients with comprehensive knowledge about the positive and negative effects of tamoxifen treatment in order to minimize these risks. It is important for healthcare providers to keep a close eye on their patients during treatment and respond promptly to any signs of illness or new symptoms.
Novel Approaches to Personalized Treatment Strategies
The treatment of ductal carcinoma in situ (DCIS) has undergone significant changes over the years, thanks to recent advances in molecular biology and imaging techniques. In the present day, oncologists are more aware of the diversity within DCIS tumors, enabling them to create more tailored treatment plans for each patient. A recent study has shown that tamoxifen may not be effective in treating ER-positive DCIS in women who have undergone surgery, as discussed in this article. This paradigm shift is reflected in the increasing use of multi-gene expression assays to guide treatment decisions. Molecular profiles of DCIS tumors are used in these assays, which can predict the likelihood of progression to invasive disease or response to certain treatments.
Integrated precision oncology is also showing promise in clinical applications. Indicators for therapeutic evaluation include novel pathways and actionable mutations that are easily targetable, while clinician-specified genomic sequencing and bioinformatic tools enable the identification of these pathways in DCIS tumors. Through this personalized approach, it is possible to identify effective therapies that are more conducive to treatment and have fewer side effects, which could result in better patient outcomes and quality of life.
Novel DCIS treatment strategies are being developed with the help of immuno-oncology. Early-stage breast cancer can be treated successfully with checkpoint inhibitors, including DCIS. The mechanism of action of these agents is to release the immune system from its restraints, allowing it to recognize and attack cancer cells more efficiently. Checkpoint inhibitors are being combined with other immunomodulatory agents or targeted therapies by researchers.
As our understanding of DCIS biology advances, so will the treatments we receive. A multidisciplinary approach is expected in the future for individualized treatment of this disease, which will involve molecular diagnostics, innovative immunotherapies, and treatments that are tailored to the individual patient's needs. By utilizing precision medicine, clinicians strive to provide more effective treatments that are less toxic and can enhance cancer outcomes and make the experience more enjoyable for all.
Evaluating Long-Term Outcomes and Future Directions
Over the past few decades, there has been a significant amount of research on whether tamoxifen is advisable for individuals with ductal carcinoma in situ (DCIS) to treat the tumor effectively for 3-5 years. Initial research yielded optimistic results, while contemporary studies have provided insight into possible drawbacks and restrictions in the application of this technique. In the process of advancing, it is imperative that we continue to assess the long-term effects of using tamoxifen therapy on DCIS patients and explore new options for treatment.
Recent research indicates that treatment decisions for DCIS patients must be based on personalized risk stratification. For example, studies have shown that women with high-risk DCIS, defined by features such as high-grade histology, large tumor size, and positive margins, may derive greater benefits from tamoxifen than those with low-risk disease. On the other hand, women who have DCIS that is less likely may experience more harmful effects from tamoxifen, including uterine cancer and deep vein thrombosis.
Efforts are being made by researchers to identify biomarkers that can predict response to tamoxifen in DCIS patients with the aim of better tailoring treatment to individual patient preferences. As an example, studies have shown that the status of the molecule at the estrogen receptor (ER) is one of many important predictors of efficacy: "[T]any type of tumor that contains an ER gene has been found to be more sensitive to tamoxifen than other drugs." Other potential biomarkers under investigation include Ki-67 expression, HER2 amplification, and genomic profiling.
We are still working on that aspect of the science behind tamoxifen and its role in DCIS, but we have many more questions to answer. Larger, longer-term studies are necessary to fully assess the drug's long-term safety and efficacy. The urgent need for alternative or combination therapies that can minimize the risk of negative outcomes while enhancing or maintaining the desired outcome is also of concern.
In order to achieve this goal, several clinical trials are currently being conducted to investigate new tamoxifen-based treatments and novel agents for DCIS treatment. The purpose of these studies is to determine the most effective methods for delivering doses, duration of therapy, and co-treatment strategies that maximize benefits while minimizing risks. The TAILORx trial is examining the use of aromatase inhibitors in women with hormone receptor-positive DCIS who are postmenopausal, and the NSABP B-39 trial is investigating whether exemestane plus one dose of tamoxifen is more effective and safe than using tamax alone.
In the final analysis, it is imperative to conduct further research on the long-term effects and limitations of tamoxifen administration for the treatment of DCIS patients. Our approach to improving patient care and outcomes can be achieved by identifying populations at risk who may benefit the most from this therapy and devising measures to minimize its negative impacts.
| Biomarker | Role in Predicting Tamoxifen Response |
|---|---|
| Estrogen Receptor (ER) Status | Predicts sensitivity to tamoxifen, with ER-positive tumors showing greater response |
| Ki-67 Expression | May predict cell proliferation and tamoxifen sensitivity |
| HER2 Amplification | Potential predictor of resistance to tamoxifen, with HER2-positive tumors potentially benefiting from anti-HER2 therapies |
| Genomic Profiling | May identify subtypes of DCIS with distinct genetic profiles and potential responses to tamoxifen-based therapy |
We recommend you read it
Read on for details about Tamoxifen and its applications other than just treating breast cancer.













