ADS:
Toremifene vs Tamoxifen - What's the Difference?
The treatment options for breast cancer are many. Toremifene and Tamoxifen are two of the most commonly used drugs for breast cancer patients that respond to hormone-receptor positive therapy. Despite their differences in how they work, both medications aim to prevent estrogen from fueling tumors and may cause adverse effects.
It is essential for women diagnosed with breast cancer to comprehend the distinctions and make an educated guess about the most appropriate treatment approach. In this article, we'll delve into the world of Toremifene vs. Tamoxifen, examining their similarities and disparities, so you can make a more educated choice.
Tamoxifen and Toremifene, both slender estrogen receptor modulators, are designed to bind specifically to specific estrogenic receptors in breast tissue. While the mechanism of action is alike and distinct among them, their chemical structures produce dissimilar pharmacological effects.
The effectiveness of Tamoxifen as a breast cancer treatment and prevention drug is widely acknowledged, with many individuals using it. The risk of invasive breast cancer is reduced by 38%, and mortality rates are reduced by 17%, as per the evidence. To prevent tumor growth, tamoxifen blocks estrogen receptors.
Tamoxifen is a newer blocker of estrogen that is similar to those found in Toremifent, another drug. However, the chemical structure of Toremifene has been developed to provide benefits that may not be available with Tamoxifen due to its potential advantages in side effect profiles and effectiveness for certain patient populations.
Toremifene and Tamoxifen are two medications that have different characteristics, with Toream Iffan containing the same dose as Tamoxetine in terms of specific dosage recommendations, dosing effectiveness, and potential benefits for certain types of breast cancer patients. With an understanding of these distinctions, you can make a more confident decision about which medication is appropriate for your specific needs and circumstances.
Toremifene VS Tamoxifen - Which Breast Cancer Treatment Is Best For You?
The prevention of breast cancer tumor recurrence is particularly effective with two drugs: Toremifene and Tamoxifen. SERMs are designed to decrease the risk of recurrence by inhibiting estrogen-containing effects in cancer. Although they have a common aim, there are important distinctions between these two drugs that could potentially make one more effective for you.
When deciding on breast cancer treatment with SERM, it's important to consider factors such as whether the woman is in her mid-twenties or getting married, and certain cancer markers. Toremifene and Tamoxifen are both medications that you can compare and contrast, so don't be confused.
- The FDA has granted approval for Tamoxifen to be used in women who are pre and post-menopausal and those with early breast cancer recurrences that express hormone receptors. However, Toremifene is only suitable for postmenopausal women.
- The effectiveness of Tamoxifen has been thoroughly researched and consistently demonstrated positive effects in reducing the incidence of breast cancer recurrence, particularly in younger age women. Although Toremifene has anti-tumor effects, the evidence supporting its use is weaker than that of Tamoxifen.
- Hot flashes, vaginal dryness, and changes in menstrual flow are common side effects of both medications, but their safety profile is uncertain. Although Tamoxifen can cause some serious cancers, Toremifene has a lower safety profile due to fewer cases of blood clots and endometrial cancer.
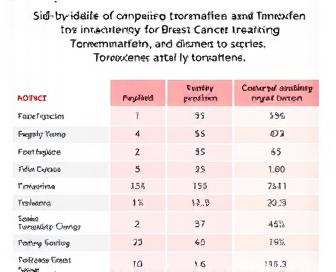
| Medication | Menopausal Status | Efficacy | Safety Profile |
|---|---|---|---|
| Tamoxifen | Premenopausal and postmenopausal | >Strong evidence of efficacy in reducing breast cancer recurrence rates | Increased risk of blood clots, endometrial cancers, and hot flashes |
| Toremifene | Only postmenopausal women | Moderate evidence of anti-tumor effects; less robust compared to Tamoxifen | Favorable safety profile with fewer reports of blood clots and endometrial cancers |
Toremifene and s. The individual factors mentioned above are essential when using Tamoxifen to treat breast cancer. The preferred medication is Tamoxifen if you're a woman going into menopause or have substantial evidence that it helps your case. Nevertheless, Toremifene may be a viable alternative for postmenopausal individuals seeking individualized advice and, ideally, with fewer risks.
Understanding the Medications
In this section, we will describe the differences between the different types of drugs to determine which is right for each case: Toremifene or Tamoxifen. They provide information on how they work (massive breast cancer), their side effect profiles, and who they are compared to so you can make an informed decision about your treatment."
Toremifene vs Tamoxifen: Mechanisms of Action
SERMs, which block estrogen activation on specific cell receptor sites, are present in both Toremifene and Tamoxifen. Their specific receptors and interactions with them differ, despite their differences.
- Due to its affinity for estrogen receptors alpha (ER), Toremifene has a better chance of binding to these receptor endpoints than Tamoxifen, which is believed to be more effective in inhibiting breast cancer cell growth.
- In contrast, Tamoxifen possesses an equal affinity for both the Erythromycin receptor (ER) and Reissineux Gramma Lupus testois (Erythemofen) as well as its Energy Resistor (Energetoxin-Receptor) receptors, which may allow more varied effects throughout the body.
Side Effects Comparison
SERMs like Toremifene and Tamoxifen can cause a variety of side effects due to their interactions with estrogen receptors. The two medications have some key differences, but many of the adverse reactions are alike.
- The cause of hot flashes is often linked to the reduction of estrogen levels in both drugs, but research indicates that Toremifene may have a greater impact on this issue.
- Vaginal discharge and bleeding: Tamoxifen tends to cause more frequent vaginal discharge and bleeding due to its higher affinity for ER receptors.
- Alterations to thyroid function have been identified for Toremifene, which may lead to a higher likelihood of developing thyroid issues such as hypothyroidism, while Tamoxifen may cause hypertheliosis in some individuals.
Patient Demographics and Indications
Understanding the patient demographics and indications for each medication can also inform treatment decisions. Despite their approval for breast cancer treatment, there are subtle variations in the recommended groups of both drugs.
- The primary indication for Toremifene is for the treatment of metastatic breast cancer that has progressed beyond initial hormone therapy, with a particular emphasis on ER-positive tumors.
- Adjuvant therapy for early-stage breast cancer, which includes premenopausal women with ER-positive disease, is often combined with Tamoxifen after surgery and radiation treatment.
Conclusion
You can choose between Toremifene and Tamoxifena by examining their mechanisms of action, side effect profiles, and patient characteristics to determine which treatment option is most suitable for your breast cancer. Take into account these factors with your physician before deciding on the appropriate measures to handle your illness.
Breast Cancer Types and Stages
The disease is complex and can affect women of all ages. It originates from the breast tissue, which comprises milk-producing glandular and glandulous structures known as ducts and guitarllary structures in lobules. Different types of cancer can be identified in breasts based on their biology and behavior.
Types of Breast Cancer
Multiple types of breast cancer exist, such as:
| Type | Description |
|---|---|
| Invasive Ductal Carcinoma (IDC) | The most common type of breast cancer, accounting for about 80% of all cases. It begins in the ducts and spreads into surrounding tissues. |
| Ductal Carcinoma In Situ (DCIS) | A non-invasive tumor that develops within the milk ducts. DCIS is considered a precancerous condition, but it can recur as invasive cancer if left untreated. |
| Invasive Lobular Carcinoma (ILC) | A less common type of breast cancer that begins in the lobules and spreads to surrounding tissues. ILC often lacks visible signs of a mass or lump. |
| Ductal Carcinoma with Medullary Features | A rare subtype characterized by large, dark tumor cells with distinct borders and a lack of lymph node involvement. |
| Tubular Adenocarcinoma | A rare type of invasive breast cancer that appears as small, tube-like structures under a microscope. |
| Mucinous Carcinoma (also known as Colloid Carcinoma) | A rare subtype characterized by a gel-like or mucus-rich stroma surrounding the tumor cells. |
Stages of Breast Cancer
Through the use of the TNM system, breast cancer can be assessed in stages by examining three primary factors:
- T4 tumors and their size.
- Lymph node status is N0N3.
- M : Distant metastasis presence (M0-M1).
The stage of breast cancer is determined by these factors, with the initial stages progressing to the most advanced stage at Stage I and Stage IV. The staggered approach helps with treatment decisions and predicts prognosis.
By understanding the various stages and types of breast cancer, it is possible to determine which treatments are most effective and which ones are least likely to result in successful outcomes. During the process of diagnosing patients, it's important to collaborate with healthcare professionals to develop a personalized treatment plan that suits their individual needs.
Toremifene vs Tamoxifen: Key Differences
Toremifene and tamoxifen are two of the many medications that are used to treat breast cancer, with the former being a selective estrogen receptor modulator (SERM) for hormonal changes in the developing breast. Although there are some commonalities between the two medications, there can be significant distinctions that may affect which one is preferred by different patients.
Dosage and Administration : Toremifene is available in oral tablets with a standard daily dose of 60 mg, whereas tamoxifen is also taken orally but comes in a variety of doses (10-40 mg per day), depending on the indication and patient factors. Because of the longer half-life of toremifene, it can be taken only once a day, while tamoxifen may need several daily doses.
Despite their similar binding to estrogen receptors in breast tissue, both SERMs display different affinity patterns. The binding affinity of toremifene is greater for alpha receptors than for beta receptors, while tamoxifen has a stronger bond with the latter. This variation could impact their efficacy and side effect profiles.
Both drugs have demonstrated significant anti-cancer effects in early breast cancer studies. A comparison of toremifene and tamoxifen found that patients with estrogen-positive tumors had similar odds of survival, but to the right, they had slightly higher chances of surviving until their second relapse occurred.
In comparison to tamoxifen, Toremifene has an improved safety profile, particularly when it comes to potential side effects on the gastrointestinal tract, such as nausea and vomiting. On the other hand, toremifene may present a greater risk of developing complications such as deep vein thrombosis and pulmonary embolism, which are rare but potentially fatal.
Toremifene and tamoxifen are two different medications, but depending on the patient's characteristics (such as age, menopause, and concurrent medical conditions), they may be prescribed together. For example, tamoxifen may be more effective in treating younger patients due to its proven long-term adjuvant benefit in preventing contralateral breast cancer; it may also be preferred by older patients who prefer toremifene for its easier dosing regimen.
Side Effects and Risks
When considering whether to use Toremifene or Tamoxifen as a breast cancer treatment, it's important to be aware of the potential side effects and risks associated with each medication. The two medicines, while generally well tolerated, may produce a range of unintended consequences that could lead to decreased quality of life. In this section, we'll delve into the common and less frequent side effects of Toremifene and Tamoxifen, as well as discuss the potential long-term risks of taking these medications for extended periods.
Hot flashes, dryness of the vagina, mood changes, and periods. Sorry Toremifene, it contains steroids. The symptoms of fatigue, joint pain, or headaches may manifest in some women, while others may experience weight gain or changes in their sex life force. On the other hand, Tamoxifen is frequently associated with more severe side effects, such as blood clots, endometrial cancer, and cataracts. Tamoxifen in women increases the risk of deep vein thrombosis (DVT) and pulmonary embolism.
Rare but potentially serious side effects include liver damage, stroke, and ovarian cancer. Rarely, Toremifene or Tamoxifen can cause severe allergic reactions or anaphylaxis. Report any unusual symptoms or concerns to a healthcare provider without delay. By conducting regular check-ups and monitoring, it is possible to detect potential issues early on, allowing for prompt intervention and treatment adjustments.
Toremifene and Tamoxifen are associated with higher rates of uterine cancer, particularly in women who have reached their 50s or 60s. If women continue taking the medication, they may experience a decrease in their bone density over an extended period, which can lead to osteoporosis or fractures in later life. When evaluating the potential benefits of these treatments, it's important to establish a clear understanding of what'll work best for you and discuss individual concerns with therapists.
Patient Selection Criteria
The patient selection process is a crucial step in determining which breast cancer treatment - Toremifene or Tamoxifen - is best for an individual. Among other things, this involves assessing the tumor type and hormone receptor status, as well as the patient's overall health condition (metabolism, blood volume, bone mineral density, and oxygen retention), age, quality of life, etc. By taking into account these variables, doctors can develop a personalized treatment plan that ensures the intervention is effective while also minimizing any potential side effects.
Treatment choice is heavily influenced by Hormone Receptor Status. Because of its proven effectiveness and safety profile, Tamoxifen is often the first line of defense against estrogen receptor (ER)-positive tumors. Nevertheless, Toremifene could be the more effective treatment option for patients with ER-positive, progesterone receptor (PR)-negative, or PR-unknown tumors, as it has been shown to have a greater impact on these types of tumors. Further investigation is necessary to determine the differences between these agents in specific patient subgroups.
The stage of breast cancer also influences treatment decisions. To manage early-stage disease (Stages I and II), patients may resort to using adjuvant medications like Toremifene or Tamoxifen after surgery, while advanced stages (III and IV) often require combination therapies such as aromatase inhibitors and/or chemotherapy. Despite being tested in phase III trials, Toremifene has demonstrated promise but still requires additional research to support its claim as a primary treatment for metastatic breast cancer patients.
Patient age can also impact the choice between Toremifene and Tamoxifen. Although both agents are approved for use in women who have experienced menstrual cycles after their period, there is little evidence of efficacy in premenopausal patients with early-stage disease. The use of Toremifene has been found to be more effective in reducing hot flashes and improving the quality of life for this population, according to some studies. However, it is still too early for research to fully explore the benefits and risks associated with these agents in women who are going through premenopause.
Making an Informed Decision
In the event that you have breast cancer treatment, it's important to make a decision about what works best for you and your circumstances. Toremifene and Tamoxifen both have their own advantages and disadvantages, which must be taken into account when weighing your medical history, personal preferences, and lifestyle. You should treat this decision as a joint effort between yourself and your doctor.
It's crucial to consider the benefits and drawbacks of each therapy if you want to have a complete understanding of the two cures. Your doctor should be the first to address any concerns or questions you may have about potential side effects, dosage schedules, or long-term consequences. This allows you to make a decision that is both wise and prudent, considering short-term health goals as well as future quality of life.
Listed below are some important points:
- Acquire knowledge about your breast cancer: Identify the classification, type, and status of hormone receptors to guide your treatment decision-making.
- Examine possible side effects: Although both drugs can cause hot flashes, night sweats, and mood swings, the incidence of these symptoms is likely to be lower with Toremifene.
- Talk about medication reactions: Make sure to tell your doctor all the prescription and OTC medicines you are taking so there are no potentially dangerous combinations.
- Observe your lifestyle: Assess how the treatment program will affect you, including your daily routine and relationships.
- Examine the merits of each drug: Toremifene, which lowers the risk of osteoporosis, may be more appropriate for women in their younger years, while Tamoxifen is frequently prescribed for older individuals who have reached menopause.
There is no one-size-fits-all treatment for breast cancer. By carefully examining your individual circumstances and consulting with a healthcare professional, you can make an informed decision that sets you on the path toward effective management and optimal well-being.
We recommend you read it
We urge you to review the following for more information on Tamoxifen and its treatment options, particularly if you are currently using one.
- Can I take ashwagandha with tamoxifen?
- Breakthrough bleeding on Tamoxifen.
- Things to know about berberine and Tamoxifen.













