Home >
Erectile Dysfunction >
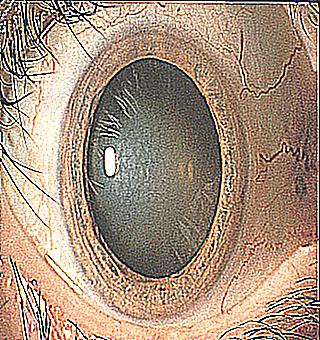
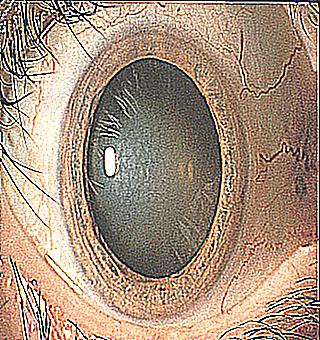
How to deal with cloudy cornea
How to deal with cloudy cornea?
Careful preoperative planning is essential to the success of cataract surgery if you have an early stage of cataract. It is important for the physician to evaluate the patient's ability to lie flat and to identify anatomical changes in the eye, such as weak areas or a shallow anterior chamber. Success depends largely on finding sources of potential complications before surgery and adjusting the approach as needed.
One of the main difficulties is the presence of corneal pathology, which causes opacity and complicates access through the cornea to the lens, increasing the likelihood of inaccurate calculations. Common causes of this type of corneal pathology include central scarring, severe corneal surface disease, limbal stem cell failure, and endothelial cell dysfunction. This article looks at the causes of cloudy corneas and provides tips to help people respond confidently to problems with corneal cloudiness.
Optimizing the ocular surface
Before performing calculations for a patient with a cloudy cornea, the doctor needs to heal his ocular surface. This step helps ensure accurate biometrics and topography readings, which can change significantly before and after treatment. In addition, treating ocular surface diseases not only improves visualization during surgery, but also reduces the risks that may arise after surgery. Most importantly, control will lead to a better overall refractive effect and higher patient satisfaction.
Less common but more serious conditions that can lead to poor visualization include Stevens-Johnson syndrome. Preoperative preventive and stabilizing measures are the key to achieving satisfactory visual results in these cases. The inflammation leads to changes, predisposing patients to lid margin disease. Since surgical manipulation can aggravate the disease process, the physician must control any superficial disease or existing inflammation.
There is a wide arsenal of tools for preparing the ocular surface for surgery. Frequent use of topical corticosteroids can be tried. However, these treatments may not be sufficient.