Home >
Erectile Dysfunction >
Male infertility symptoms and treatment
Male infertility - symptoms and treatment
The process of creating spermatozoa (spermatogenesis) occurs in the testicle. The process of creating one sperm cell takes about 70 days.
The process of creating spermatozoa is stimulated by follicle-stimulating hormone (FSH), which is produced in the pituitary gland in the brain. In the absence of FSH, spermatogenesis does not proceed, and spermatozoa are not formed.
Spermatogenesis is a rather delicate process. Many factors can disrupt its normal course (increased scrotal temperature, taking medications, X-rays) and lead to the creation of spermatozoa with an irregular structure (morphology), poor mobility and defective genetic material that are not capable of fertilization.
As a result of the passage of the epididymis, which takes about a week, spermatozoa improve their mobility, and there is also a change in the molecules on the surface of the spermatozoon necessary for interaction with the egg.
Against the background of inflammatory processes in the epididymis, the process of maturation of spermatozoa may be disturbed, and they will not be able to fertilize the egg. In some cases, as a result of an inflammatory process or after operations on the epididymis, an obstacle is formed for the passage of spermatozoa, as a result of which they do not enter the sperm.
After passing through the epididymis, spermatozoa can be stored in a man's body for several weeks, retaining the ability to fertilize. But if the sperm is stored for too long, the spermatozoa begin to degrade and die.
Destroying sperm can damage new sperm, preventing them from leaving the epididymis. Men are advised to ejaculate every two or three days to keep sperm quality in optimal condition.
During ejaculation, about 250 million sperm begin to move out through the vas deferens and urethra (urethra). The movement of spermatozoa is provided by the contraction of the muscles of the vas deferens and the urethra, which are accompanied by pleasant orgasmic sensations. As a rule, sperm ejection occurs in several portions. Most spermatozoa are contained in the first portion, the second and third contain mainly the secret of additional male gonads - the prostate gland and seminal vesicles.
The secret of the accessory gonads (prostate and seminal vesicles) is necessary to ensure the vital activity of spermatozoa after ejaculation. With an inflammatory or other pathological process in the prostate or seminal vesicles, the composition of their secretion may change, which disrupts the functioning of spermatozoa and reduces the likelihood of conception.
After entering the vagina, the sperm must leave it within a few minutes and move to the cervix. The fact is that the environment of the vagina is acidic, which is necessary to protect the female body from bacteria and viruses. However, the acidic environment quickly destroys spermatozoa, if the spermatozoon is in it for more than two minutes, it dies. According to statistics, only one in 100 spermatozoa manages to leave the vagina and move to the cervix.
In this regard, it is very important that sperm During ejaculation fall as close to the cervix as possible, which is impossible with such anomalies as hypospadias (the external opening of the urethra is located on the lower surface of the penis).
The cervix contains a special mucus, which, on the one hand, protects spermatozoa from the aggressive environment of the vagina, on the other hand, it can prevent their further movement. The consistency of the mucus depends on the hormonal status of the woman, and most of the time it is impermeable to even the healthiest and most mobile spermatozoa. A few days before ovulation, the consistency of the mucus changes in such a way that it becomes able to skip sperm.
In some cases, cervical mucus may contain antibodies (proteins produced by the immune system to fight foreign substances that have entered the body) to spermatozoa, which do not allow spermatozoa to pass cervical mucus even during ovulation.
In this situation, the woman's body comes to the aid of the sperm
It is very small, only a few sperm heads in diameter, so sperm that move randomly will not be able to enter it. This stage is overcome only by spermatozoa with fast and rectilinear movement.
They can stay in this state for quite a long time - about 48 hours.
They begin intensive movements with their tail, detach from the wall and quickly move towards the egg. At this stage, 6-8 spermatozoa will remain, and they have several hours to fertilize the egg, since the life span is very short.
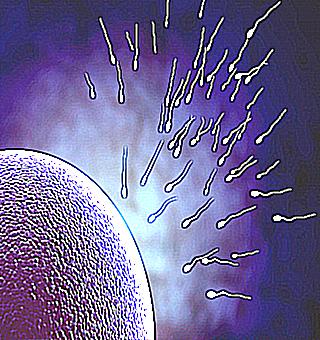
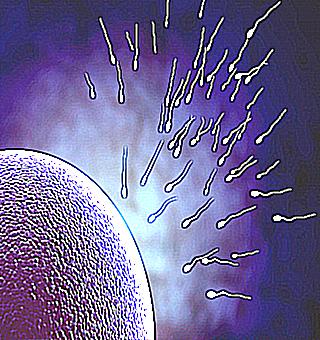
Compared to the sperm, the egg is a rather large cell, the largest in the human body.After leaving the ovary, it is surrounded by a cloud of cells called follicular cells, through which spermatozoa must penetrate before they come into contact with the surface of the egg
After passing through the follicular cells, 1-2 sperm reach the egg, which need to get inside. To do this, the spermatozoon has an enzyme sac at the very top of the head, which bursts as soon as the spermatozoon comes into contact with the outer surface of the egg. These enzymes help to dissolve the outer membrane of the egg and, combined with the powerful movement of the tail, help the sperm enter the inside of the egg. As soon as the sperm gets inside, the egg membrane changes its chemical properties and becomes completely impermeable to the rest of the sperm. After the fusion of the sperm with the egg, an embryo is formed, and the development of pregnancy begins.
If a spermatozoon is functionally immature and does not contain the necessary signaling molecules on its surface, it will not be able to make contact with the egg and fertilization will not occur. There is a rare anomaly - globulozoospermia, when spermatozoa do not have a conical, but a round head. The reason for this is the absence of a sac with enzymes (acrosomes), which also prevents the penetration of the sperm into the egg.