ADS:
Medicines for prostate treatment:

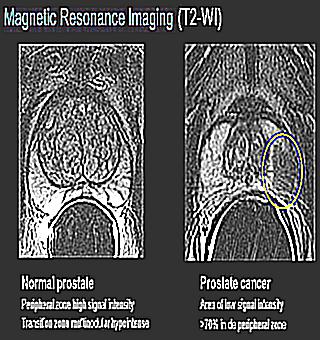
In the diagnosis of prostate diseases, the role of MRI is especially great. In economically developed countries, prostate cancer occupies one of the first places in the structure of oncological diseases, so the interest in methods for its early detection is especially great.
MRI is most often used for the detection and differential diagnosis of Prostate cancer, as well as for the diagnosis of other diseases of the prostate and seminal vesicles.
Let's consider some diseases of the prostate gland and seminal vesicles detected by MRI examination of the pelvis:
This is an adenomatous enlargement of the transition zone of the prostate. Typically occurs in men over 50 years of age, most often progresses over time. Clinically manifested by dysuric phenomena, weakening of the urine stream, chronic urinary retention.
Rarely causes prostate cancer.
A) T2-tra b) T2-sag The zonal anatomy of the prostate is well visualized, pronounced hyperplasia of the transition zone of an inhomogeneous structure, compression of the peripheral zone against this background. The transition zone protrudes into the lumen of the bladder (b).
Adenocarcinoma is the most common malignant tumor of the prostate, usually occurring in the peripheral zone. In men, it is the most common malignant tumor. Clinically, an asymptomatic course is characteristic for a long time; palpation, as a rule, only large, peripherally located tumors are determined. Urinary retention, infravesical obstruction - late complications of adenocarcinoma. Deterioration of the general condition in patients occurs with metastatic prostate cancer.
The frequency of occurrence increases with age. Screening, including determination of the level of PSA and digital rectal examination of the prostate, should begin at age 50.
A) T2-axial image b) T2-coronal image.
Male, 62 years old. Verified prostate cancer. In the posterior-lateral sections of the peripheral zone of the left lobe of the gland (on the border of the central and apical parts of the prostate), an area of pathologically reduced MR signal is visualized. The intact capsule of the gland is preserved (stage T2a).
T2-VI, axial plane. Ca (cancer) is a small focus of a pathologically reduced MR signal.
The area of the pathologically reduced MR signal is determined in the peripheral zone of the left lobe of the prostate (the central part of the gland). In this case, a violation of the integrity of the capsule of the prostate gland (T3a stage) is visualized.
A) T2-cor b) T2-tra c) T1FS din+C
A large tumor of the right lobe of the prostate gland with invasion of its capsule, spreading to the paraprostatic tissue (arrows) is determined. With intravenous dynamic contrast (c), a pronounced, diffusely inhomogeneous enhancement of tumor tissue is determined in the arterial phase.
A) T2-axial image b) T2-coronal image
The tumor of the left lobe of the prostate is determined with signs of spread to the base of the left seminal vesicle (arrows, b).
Acute prostatitis is an acute inflammatory process in the prostate gland, characterized by signs of general intoxication, pain in the perineum and inguinal region, as well as painful sensations when emptying the bladder and frequent urge to urinate (especially at night). The pain syndrome leads to difficulty urinating, sometimes to acute urinary retention.
In some cases, whitish or colorless purulent discharge from the urethra is possible.
Male, 45 years old. Acute prostatitis. On the presented tomograms in T2-WI, the axial plane (a) and T2 with fat suppression in the coronal plane, an increase in the volume of the peripheral zone, its swelling is determined.
The reason for the formation of a prostate abscess is pathogenic bacteria that caused the development of prostatitis, and in the case of a hematogenous abscess, bacteria that contributed to the development of the main focus of infection in the body.
The following forms of prostate abscess are distinguished:
Prostate abscess is characterized by all the symptoms of prostatitis, but to a greater extent. The general condition is severe, the temperature is high with chills, tachycardia, profuse sweating. Sharp, pulsating, unilateral (because an abscess often affects one side of the organ in isolation), pain radiating to the rectum is characteristic.Pain syndrome leads to difficulty in defecation and urination, including acute urinary retention. In the event of an abscess rupture, cloudy urine is noted, or the presence of pus in the feces.
A) T2-tra b) T1-tra+C c)DW
On the T2-axial image (a), an irregularly rounded focus of increased MR signal intensity in the central zone of the left lobe of the prostate gland is determined. With intravenous contrasting (b), there is a peripheral enhancement of this focus (capsule), with non-contrasting central sections. On the diffusion-weighted image, signs of diffusion limitation from a given cavity formation (abscess) are determined.
35. Male, 31 years old with infertility. The T2-axial image shows the absence of the left seminal vesicle in the presence of the left vas deferens (arrows).
The presence of cysts in the seminal vesicles in autosomal dominant polycystic kidney disease is of great clinical significance. With ultrasound, this pathology can be erroneously interpreted as prostate cysts.
The clinical picture of polycystic disease may include hemospermia.
On the presented T2-WI with fat suppression, bilateral cysts of the seminal vesicles (a, axial plane) and enlargement of the kidneys due to multiple cysts (b, frontal plane) are determined.
37. a) T1-tra FS b) T2-tra c) T1-tra+contrast
Man, 31 years old. Hematuria. A cavitary inclusion of an irregularly oval shape is determined in the projection of the left seminal vesicle, which has signal characteristics different from liquid (hyperintense MR signal in T1-WI, a - a sign of hemorrhage). With intravenous contrast (c), there is no peripheral enhancement, which indicates the absence of infection of the cyst.
38 a) Т1-tra+С b) Т1-cor+С
Man, 78 years old. In the projection of the left seminal vesicle, a cystic inclusion is determined with non-bumpy contours and signs of peripheral contrast enhancement of the capsule (a festering cyst-abscess).
Müllerian duct cyst is more common in boys with hypospadias and in intersex people. Sizes vary considerably. Clinically, they often do not manifest themselves in any way, but in some cases there may be discomfort in the perineum, dysuria, hematuria, urinary retention, urinary tract infections, epididymitis, oligospermia.
38. Male, 72 years old with prostate cancer. Large cyst of the Mullerian duct. A fluid inclusion is seen between the rectum and the prostate in the midline. For such a cyst, localization along the midline is typical, which makes it possible to differentiate it from a seminal vesicle cyst.
Vesiculitis is an inflammation of the seminal vesicles. Clinically characteristic is the appearance of pain above the pubis and in the perineum, which radiate to the lower back, groin or sacrum. Pain is aggravated by defecation and urge to urinate. During defecation, there is also a discharge of mucous contents from the urethra, sometimes with streaks of blood, this is the secret of vesicles. In addition, with vesiculitis, ejaculation becomes painful and traces of blood appear in the semen. There is an erection disorder. The general condition also suffers: weakness, headache, increased fatigue and temperature are characteristic. The accompanying symptoms of prostatitis are often exacerbated.
40 a) T2-tra b) T1-tra + contrast
Man, 34 years old with hematospermia. Pre-contrast T2-WI (a) and post-contrast T1-WI images (b) in the axial plane demonstrate diffuse thickening of the walls of the seminal vesicles, heterogeneity of their internal structure.
3 721 Elena Polyakova, doctor
(1 vote, average: 5 out of 5)
Magnetic resonance imaging (MRI) of the prostate is a diagnostic method for confirming or refuting prostatitis, adenoma, abscesses, and cancer. When scanning, the structure, size, position of the organ is determined, abscesses, inflammation, benign and malignant tumors are detected. The accuracy of diagnosis is more than 89%, which is higher than with ultrasound or CT. If you combine an MRI with a biopsy, then the figure reaches 100%.
Method of MRI of the prostate gland is a translation into a picture of the resonant reaction of hydrogen from tissues to a magnetic field. The radiated energy is captured in the radio frequency range and displayed on the screen. The resulting picture gives detailed information about the discreteness, topography, size, outlines of the prostate. These parameters are needed to determine urological pathologies: MRI can show inflammatory, proliferative, oncological diseases of the prostate.
A man is referred for an MRI only after simple procedures (this is due to the complexity and high cost of the service).For example, the diagnosis of chronic prostatitis begins with the collection of anamnesis, rectal examination, laboratory blood and urine tests. If the measures taken did not allow to accurately establish the disease, the patient is given a referral for magnetic resonance imaging.
In addition to differential diagnosis, an indication for MRI is the study of the prostate in the preoperative period. The study will show the degree of damage to the organ and the involvement of neighboring structures (tissue, bone, blood, nerve) in the pathological process. From the pictures, the doctor will get an accurate idea of what exactly during the operation should be removed from the man.
Australian scientists from the Wesley Institute have done a lot of scientific work comparing the effectiveness of four types of instrumental examination: ultrasound, TRUS, conventional tomography and MRI-guided biopsy of the testicles, bladder and prostate. 489 patients with elevated PSA were studied. The subjects, with their consent, underwent all four types of diagnostics. Prostate cancer was found in 234 people.
The biggest inaccuracy according to the results of the study was found in the ultrasound examination - cancers were detected only in 62%. TRUS is more precise - it helped to detect oncological formations in 77%. MRI accuracy without biopsy - 89%, with biopsy - 100%.
The paradox is that, despite the minimal probability of a false diagnosis, MRI is much more likely to do ultrasound and TRUS. The reason is the large number of contraindications and the high cost of tomography.
Foods that increase gas formation are excluded (mineral water, beans, beans, kefir). A prerequisite is not to eat at all for 4 hours before the MRI.
Prostate MRI is always performed with an empty rectum. The patient prepares for the procedure on his own: 12 hours before the procedure, it is recommended to cleanse the intestines (drink a laxative or make an enema). Psychological preparation for the study is based on the fact that the patient should tune in to immobility in the supine position for more than half an hour. The examination does not cause any discomfort (pain, burning).
According to medical standards, magnetic resonance imaging is performed before transrectal excision of prostate tissue (the break between procedures does not play a role - it can be done within one hour). This method is called fusion (fusion) prostate biopsy - it is done under MRI control.
Plus the "double" procedure - doctors do not take the material "blindly" (from random areas of the prostate), but aimingly (from those areas that the magnetic resonance imaging scanner shows as suspicious). As a result, the number of points for taking tissue samples is reduced, which significantly reduces the risk of complications. For comparison: during a standard tissue sampling, it is performed through 30-40 punctures, when combined with an MRI - 10-12.
If the procedure is violated, tissue material was taken before instrumental diagnostics, then MRI can be done no earlier than 25 days after prostate biopsy. During this time, the wound left after the introduction of the needle into the gland will have time to heal completely.
A man can use the pajamas provided by the clinic or wear his own clothes during the procedure if they do not constrict the body and do not have metal elements.
In case of prostatitis, cancer, prostate abscess or prostatic hyperplasia, only the pelvic area should be examined, so the person is not completely placed in the device - the head, shoulders, arms remain outside the tomograph. This allows the patient to keep his eyes open, listen to music, read a book (the main thing is not to move the lower part of the body during radiation).
For an MRI of the prostate, a man is not completely placed in the apparatus - the head, shoulders, arms remain outside the tomograph.
The duration of an MRI is from 30 to 70 minutes. During the procedure, 10-20 shootings are carried out. When the scan is done, the patient needs to lie as still as possible. In the periods between them (breaks last no more than 2-3 minutes), you can move your legs a little, about which the doctor will inform you additionally.
The simplest type of MRI is an examination without the use of a contrast material. It is rarely used due to the high probability of missing cancer. The only case when it is done is the presence of contraindications for the use of contrast:
The advantages of non-contrast MRI are the reduced cost of the service, the exclusion of the likelihood of an allergic reaction. Minus - without contrast, it is more difficult to recognize areas of oncological formations.For example, in the case of small cancerous tumors in the prostate, the probability of their detection is 78%, since there are no changes in the surrounding structures.
MRI with a contrast agent is performed to determine the parameters of the prostate and to detect tumors of any size. As a contrast, use:
The products listed contain gadolinium salts. It is a metal that has a silvery tint and is clearly visible on contrast-enhanced MRI of the prostate. The drug is administered by injection (an injection is made with a syringe into a vein). In 2-3 minutes, blood with contrast reaches the prostate, and magnetic resonance imaging can be performed. A day after the procedure, the contrast agent is excreted from the body along with urine.
To improve the accuracy of diagnosis, an algorithm for multi-parameter analysis of tomography data has been developed. Another name for the system is PIRADS (Prostate Imaging Reporting and Data System). The study itself takes place on standard equipment (nowadays targeted MRI is often used, which is an examination of the prostate on an ultra-high-field tomograph).
Multiparametric MRI of the prostate takes longer than standard tomography (by 20-30 minutes). The time for analyzing the information received is also extended.
The advantage of multiparametric MRI is the ability to perform the procedure without a biopsy. The probability of "overseeing" the tumor is reduced by 12% compared to traditional magnetic resonance imaging.
An indication for an MRI is an elevated PSA in the blood. An increase in the level of antigen occurs with prostate adenoma, purulent prostatitis, bladder abscess and cancer. Magnetic resonance imaging will determine the exact pathology.
During the diagnosis, prostate cancer is confirmed if dense clots are detected on the image, which should not be present here according to the anatomy of the gland. MRI allows you to determine the form of oncology: whether the tumor is adenoid, mucinous or fibrous. For example, a weak resonant signal is characteristic of prostate cancer formed by cells with mucin (this information helps determine the appropriate type of treatment for a cancer patient). To understand the nature of the tumor (malignant or benign), a biopsy is done after magnetic resonance imaging.
Analysis of MRI data is the task of a diagnostician and a urologist. If you wish, you can use medical standards that allow you to independently analyze the images.
It is imperative to ask a specialist for an interpretation of the MRI results (an accurate diagnosis is made according to the results of MRI, PSA, ultrasound, etc.). You yourself can incorrectly decipher the data of the images and start the wrong treatment (or consider yourself healthy, do nothing and start the disease).
The main disadvantage of tomography is that it is not included in the list of services that are done free of charge under an insurance policy. The price of MRI is quite high (compared to other diagnostic methods) - this is justified by the complexity of the procedure, expensive equipment, and highly qualified personnel.
Prostate cancer is the most common type of malignant neoplasm among men. The effectiveness of the treatment of this disease today is very high, the only prerequisite for successful treatment is timely diagnosis. MRI of the prostate allows you to very quickly and accurately determine even the smallest neoplasms in the prostate gland and their nature.
Types of prostate MRI
Magnetic resonance imaging is one of the most modern methods for diagnosing various diseases, including those in the prostate gland. According to the results of its implementation, the doctor will have access to the most detailed layer-by-layer image of this internal organ. In addition, it should be noted that this is the most accurate and at the same time the safest method for detecting pathologies in the body.
The principle of the technique lies in one of the properties of hydrogen - to appear under the influence of a certain kind of magnetic rays.The patient is laid down and placed in the zone of electromagnetic radiation. It should be understood that, unlike radiation, it does not have a negative effect on the body.
In our country, it so happened that if prostate cancer is suspected, the doctor prescribes a referral to the patient for an MRI scan of the pelvis, and this is not entirely correct and appropriate. These two types of tomography are fundamentally different from each other. Having made an MRI of the pelvic organs, the doctor will see a generalized picture, and with an MRI of the prostate - only this organ. In the latter case, the picture will be more accurate and detailed.
Prostate MRI with Toshiba
In addition to the standard MRI method, in the case of prostate diagnostics, there are several more methods that allow you to get an even more accurate examination result:
Tomography of this organ is usually carried out in order to confirm or refute suspicions of the presence of malignant neoplasms in it. If cancer is detected, its degree and place of spread (within the prostate gland or beyond it as well) is also determined. In addition, magnetic resonance imaging may be prescribed in order to identify:
This procedure requires some preliminary preparations from the patient. In particular:
Three days before the examination, you should follow a diet, refusing to eat foods that provoke increased gas formation; if a coil MRI is scheduled, a cleansing enema should be given on the day of the MRI. Description of MRI of the prostate
The doctor must instruct the patient on the specifics of the examination and give recommendations on how to prepare for it.
The patient also needs to be aware of the existence of a number of contraindications and limitations to magnetic tomography:
MRI of the prostate is a method for diagnosing diseases of this organ, which has been used for quite a long time and actively. This is especially true for Western European countries. Among its undoubted advantages are three important factors in which it has no equal:
If we talk about the shortcomings, then first of all it is impossible not to note the high cost of such a procedure. It is unlikely that it will be possible to make it cheaper, because, firstly, the equipment itself is incredibly expensive, and secondly, only a highly qualified narrowly specialized specialist can carry out the procedure, which are very few, and thirdly, the duration of the procedure itself is up to 30 minutes or more.
In our country, the practice of free MRI examinations for privileged categories of citizens has been introduced, however, huge queues on these lists sometimes make you wait for months for the day of your examination, and in cases with diseases such as cancer, delay is unacceptable.