Home >
Erectile Dysfunction >
Autoimmune pancreatitis associated with prostatitis
Autoimmune pancreatitis associated with prostatitis
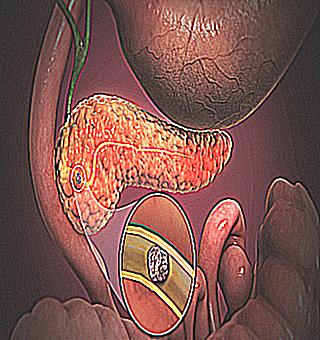
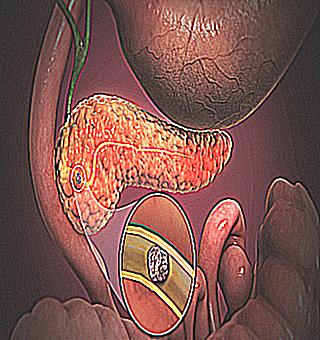
Pancreatitis is an inflammatory process that occurs in the pancreas, as a result of which the local production of enzymes and hormones is disrupted. In the process of the development of the disease, an adverse effect of enzymes occurs, whereby the tissue of the pancreas is destroyed. Simply put, the enzymes that are called upon to digest food, "digest" the pancreas itself. Any, even minor inflammatory processes of the pancreas affect the gastrointestinal tract.
There are several forms of the disease
The pancreas has the following functions
Endocrine function is responsible for the release of hormones such as insulin and glucagon, which are designed to control carbohydrate metabolism.
With proper exocrine function, the pancreas synthesizes 1.5-2.5 liters of electrolyte fluid - pancreatic fluid for transferring enzymes into the duodenum.
Also, this function serves to release such enzymes into the lumen of the duodenum:
- amylase, which helps break down starch,
- lipase, which helps the body digest all lipids,
- proteases that break down proteins.
If the pancreas does not have pathological changes, then the required number of enzymes is produced. As a result, food is perfectly absorbed and nutrients through the blood enter all cells of our body, providing it with building materials. The energy level also increases, the cells function correctly and are renewed. A person is not susceptible to disease, because the immune system receives the necessary amount of nutrients.
When there are no abnormalities in the functioning of the pancreas, therefore, the breakdown of proteins, fats and carbohydrates occurs equally well and correctly, food is processed without problems, regardless of what food a person eats. Based on this, it is a healthy pancreas and the correct functioning of the exocrine function that indicate the absurdity of the theory of separate nutrition. After all, you do not need to eat separately, as enzymes are prepared for processing absolutely any incoming food.
But there may be deviations in the functioning of the pancreas. Malfunction is observed in inflammatory processes of the pancreas. The inflammatory process can be acute or chronic. Hence the corresponding diagnoses: acute and chronic inflammation of the pancreas.
When the pancreas is inflamed, there are abnormalities in the formation of pancreatic juice, which is involved in the processing of food, the transfer of enzymes, and the synthesis of hormones.
In case of deviations in the formation of digestive enzymes, the food that a person eats is poorly broken down, not digested, and decay processes are triggered. In this case, food will be a substrate for the development of pathogenic microorganisms, which release in large quantities toxic substances of their vital activity. Accordingly, the number of toxins will increase, which will enter the body through the blood and spread through it. Deviations in the work of exocrine functions can contribute to severe intoxication of the whole body, as a result of which a person's immunity is weakened and many diseases develop, the appearance of which most doctors do not even associate with the diagnosis of pancreatitis.
First of all, the liver will suffer, which is the main filter of our body. Toxins can also enter the brain, resulting in migraines and headaches
The appearance in a man of such a disease as prostatitis is also the result of pancreatitis and an increase in the number of toxins in the body. In order to contribute to the cure of the disease, it is necessary to bring the exocrine function of the pancreas to normal and restore the normal process of digestion.
Prostatitis is an inflammatory process that occurs in the prostate gland. Any man can face this disease. The disease has negative consequences: impotence, infertility, prostate cancer. Prostatitis affects about eighty percent of men, and often the disease is not accompanied by any symptoms.
Risk factors for the onset of the disease
- The risk of inflammation of the prostate gland increases with hypothermia, a history of venereal and urological infections, which are accompanied by stagnation in the tissues of the prostate gland.
- Hypothermia of the body (single or permanent).
- Sedentary lifestyle. It can be a profession that makes a man sit for a long time.
- If a man suffers from constant constipation.
- Deviations from the norm of the rhythm of intimate life (quite frequent intimacy, or vice versa, long abstinence, incomplete ejaculation).
- The presence of chronic inflammatory diseases (pancreatitis) or chronic foci of infections in the body (untreated caries, laryngitis).
- If the patient has ever suffered from urological infections (urethritis, cystitis), or sexually transmitted diseases (chlamydia, trichomoniasis, gonorrhea).
- Conditions that can cause suppression of the immune system (chronic stress, unhealthy diet, lack of vitamins, regular lack of sleep, too much stress in athletes).
- The risk of inflammation of the prostate gland increases with chronic poisoning of the body with alcohol, nicotine, drugs).
According to the results of studies in the urological field, it has been proven that the cause of the onset of the disease can be a chronic injury to the groin (vibration, shaking), which can occur in motorists, motorcyclists and cyclists. Nevertheless, most doctors believe that all of the above factors are not the true causes of the disease, but only contribute to the aggravation of latent inflammation in the tissues of the prostate gland.
The main role in the development of the disease is played by stagnation in the tissues of the prostate gland. In case of impaired capillary blood flow, a stronger fat peroxidation, edema, exudation of prostate tissue occurs, and a favorable environment for the development of infection is formed.
The state of the intestines will not be the last place in the appearance of all kinds of abnormalities in the work of the prostate
In the body of a healthy person, the full functioning of the intestines and bladder consists in their gradual filling and periodic emptying. Changes in the size of these organs contribute to a change in their pressure on the prostate gland and its slight displacement, since these organs are quite close to each other. This will be a kind of stimulus for the prostate gland to perform its functions.
The level of filling of the intestines and bladder will be a kind of mechanical stimulus, and when this level changes, the secretion of the prostate gland is stimulated, which contributes to the complete release of the prostate ducts. In addition, actively working organs attract additional blood, which has a positive effect on the tissues that are located near them.
Abnormalities in the work of the intestines affect the condition of the prostate only when they occur for a long time (3-5 years) and have rather vivid symptoms. So, an intestinal infection that lasts a week does not affect the prostate gland, and constipation, diarrhea, or their alternation over the years can cause prostate upset and increase the risk of disease.
The above-described deviations can be caused by some diseases of the body: hemorrhoids, intestinal neoplasms, cholecystitis, pancreatitis
It should be noted that constipation will have a more detrimental effect than diarrhea, since with congestion in the intestine and its strong fullness, the prostate gland is compressed, while its blood supply and secretion of the prostate gland becomes difficult.
Abnormalities in the functioning of the bladder have less effect on the functioning of the prostate, this is due to its location and the area of contact with it.
Not so long ago, experts suggested that autoimmune pancreatitis is a systemic disease, which is characterized by an increase in plasma levels of IgG4. Other inflammatory processes can occur at the same time, for example, inflammation of the prostate gland and sclerosing cholangitis.
In order to identify the clinical pathological characteristics of pancreatitis associated with autoimmune prostatitis, specialists calculated the degree of expression of class G immunoglobulins (IgG1, IgG2, IgG3, and IgG4) in 6 men who have such a disease as autoimmune pancreatitis from prostatitis
For control purposes, ten men were analyzed in whom histological analysis of the prostate gland showed focal inflammation.
All men in the study group were found to have symptoms of autoimmune prostatitis, and the clinical picture of LUTS improved significantly after steroid treatment. Four out of five men from the experimental group showed an increase in the size of the prostate gland on digital rectal examination. Histological analysis of the prostate gland revealed lymphoplasmic and eosinophilic infiltration, as well as obliterating phlebitis in combination with atrophic processes of the prostate and fibrosis.
IgG4-positive cells compared to mononuclear cells were observed in a greater number in the experimental group than in the control group (P 0.0011).So, we can conclude that prostatitis associated with such a disease as pancreatitis can be perceived as an independent clinical pathological condition.
Prevention of prostate inflammation is the elimination of risk factors for the occurrence of the disease. A man should avoid hypothermia, periodically change a seated position to physical activity, and eat regularly and fully. If you are concerned about constipation, you need to take laxatives. In addition, intimate life should be normalized. In case of symptoms of urological or sexually transmitted infections, it is necessary to consult a doctor promptly.