Home >
Erectile Dysfunction >
Examination of the prostate and seminal vesicles
Examination of the prostate and seminal vesicles
Prostate ultrasound
According to medical statistics, prostatitis, erectile dysfunction, prostate adenoma have ceased to be age-related diseases. The "second male heart", as the prostate gland is otherwise called, does not withstand the totality of negative factors affecting a man, which include:
- hypodynamic lifestyle;
- malnutrition;
- unstable intimate relationships;
- bad habits;
- regular stress.
In addition, many men do not seek medical help in a timely manner. Diseases continue to progress and "get younger". To prevent the development of serious complications, you should regularly visit a urologist or andrologist (male health specialist), and, if necessary, undergo a simple prostate ultrasound procedure.
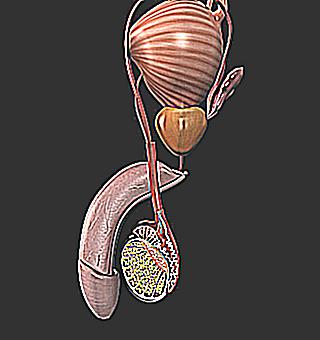
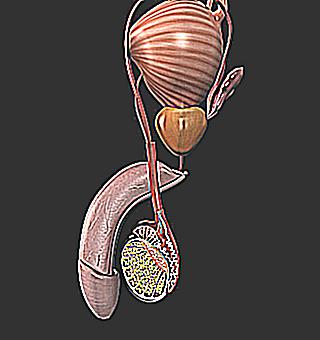
Shortly about the "second male heart"
To understand how an ultrasound of the prostate is done, you need to understand a little about the anatomy of the gland. The prostate is a small, unpaired gland of external secretion. Depending on the size of the man, its weight ranges from 25 to 55 grams. The structure of the body consists of muscle and glandular tissue. The prostate includes three parts: identical right and left parts, consisting of 30-50 scanty lobes and the anterior part, where the vas deferens and the urethra are located.
The organ is used to produce a secret containing immunoglobulins, enzymes, vitamins and acids. This substance is the basis of sperm. The prostate gland begins to function fully by the age of majority of a young man. The decline in performance, as a rule, is observed at the age of 50+. Above the gland is another important organ of male health - Seminal vesicles or vesicles. They protect spermatozoa, participate in the production of seminal fluid and disposal of its residues.
Study Purpose
Prostate ultrasound is done with previously diagnosed pathologies of the organ in order to control the dynamics of treatment, as well as the symptoms that the patient presents. The direction for ultrasound is given by a urologist or andrologist. Diagnostics is assigned in the following cases:
- inability to conceive (infertility);
- incontinence (urinary incontinence);
- unstable erection or erectile dysfunction;
- regular pain in the perineum;
- unstable emptying of the bladder (pain when urinating, decreased amount of urine, the need to strain the muscles during the process itself, frequent false urge to urinate);
- purulent or blood clots in urine or semen;
- kidney dysfunction;
- cystitis and urethritis (inflammation in the bladder and urethra);
- deviations from the norm in urine tests, PSA (prostate specific antigen and spermograms);
- hyperplasia (adenoma) and chronic prostatitis (inflammation) of the prostate.
Ultrasound diagnostic methods
Prostate ultrasound is performed in two ways. Transabdominally. This type of procedure is usually done as part of an abdominal ultrasound, through the anterior wall of the peritoneum. There are no contraindications for carrying out. Transrectal. In this case, the ultrasound transducer is inserted through the rectum. Contraindications are: hemorrhoids in the acute stage and the postoperative period after intestinal surgery. The second diagnostic option is more informative, since the proximity of the sensor to the prostate is higher. This allows a detailed assessment of changes in the gland. In addition, rectal ultrasound makes it possible to take biomaterial for differentiated diagnosis of cancer.
Preparations
Before a transabdominal ultrasound of the prostate, a man must fulfill the following preparation conditions. Two days before the procedure, eliminate carbonated drinks and kvass from the diet, as well as foods that provoke intense gas formation (beans and peas, pastries and black bread, cabbage, sweets). On the eve of the study, take carminative drugs (Espumizan, activated charcoal). On the day of the test, do not have breakfast, two hours before the diagnosis, drink at least 1.5-2 liters of water and do not empty your bladder.
The last condition must be observed for better visualization of the prostate gland. The rules for preparing for transrectal ultrasound (TRUS) are more stringent. This is due not only to the medical need to obtain objective results, but also to the patient's comfortable state of health. With regard to diet, before TRUS, you must follow the same dietary rules as before a transabdominal examination. Next:
- Carminative medication should be started two days in advance.
- In the evening, before the procedure, you should have a light meal for dinner, but no later than 19 hours.
- 2-4 hours before the procedure, an enema is performed with plain water, with a volume of about two liters. As an alternative, the Microlax enema is used.
- The bladder is filled in the same mode as with a conventional ultrasound.
Performing the procedure
Ultrasound is most often scheduled in the morning. The method of conducting is determined by the doctor.
Transabdominal ultrasound diagnostics
The patient is in a horizontal position on the back. The abdomen and the sensor of the device are treated with a medical gel. A picture of the internal organs is displayed on the monitor. With the help of a special program, the main dimensions of the organ are measured, its structural and contour parameters are evaluated. The time interval is a quarter of an hour.
Transrectal method
A man is being examined in a position on his left side, with his knees drawn up to his stomach. A thin rectal probe placed in a condom is slowly inserted into the rectum, approximately 9-11 cm. A biopsy (tissue sampling) is performed under the control of the image of the internal organs on the monitor. The duration of the procedure without a biopsy is about half an hour, and with the analysis of a biopath a little more.
Extra
With a standard prostate exam, the doctor may prescribe an additional ultrasound of the seminal vesicles and examination of the scrotum. This is necessary if you suspect inflammation of the testicle (orchitis), inflammation of the testicle and its epididymis (orchiepididymitis), expansion (enlargement) of the veins of the spermatic cord (varicocele). A man is given a protocol with ultrasound diagnostic indicators, according to which the doctor who sent him for ultrasound (TRUS) makes the final diagnosis.
Decode results
The results are deciphered by comparing the data obtained with the standards, according to the age of the man. The main parameters for assessing the organ and the norm: the shape of the prostate gland is round (rarely triangular), the lobes are symmetrical, the outlines are clear, not blurry, without pronounced bulges, the structure is granular homogeneous (homogeneous), the vessels are without abnormal changes (narrowing, expansion) .
Next, the dimensions of the prostate are analyzed:
- Width, length, thickness must correspond to digital values: 40 mm, 45 mm, 25 mm.
- Upper anterior size, anteroposterior, transverse: 24-41 mm; 16-23 mm; 27-44 mm.
Seminal vesicles are normally no more than one millimeter.
Signs of pathological changes in diseases: the presence of inclusions and an increase in the size of the gland - signs of prostate adenoma, increased conductivity (echogenicity) - inflammation (prostatitis), the absence of smooth outlines against the background of an increase in lymph nodes - an assumption of oncology (for confirmation / refutation, biopsy results are needed ). According to the bladder, the organ should not contain foreign substances (sand, stones). The norm of wall thickness is from 3 to 5.2 mm.
Prostate volume
The volume of the prostate gland is calculated according to the Gromov formula, which takes into account the age of the man (in the graphical formula, this indicator corresponds to the letter B). V0.13*B+16.4. The maximum value is V30. An increase in volume always indicates serious violations. In case of severe disorders, the urologist prescribes conservative treatment with medications.
If the ultrasound shows serious changes, an additional examination is carried out, a consultation with the surgeon is scheduled. In this case, the issue of surgical intervention is decided. Do not be afraid of a rectal examination, it is painless. This is evidenced by the reviews of men who have successfully completed TRUS. With timely diagnosis, diseases of the "second male heart" are successfully treated. Ultrasound is the only informative option.
Obtaining and analyzing prostate juice, examining the accessory gonads and their secretion.
In acute urethritis and acute inflammation of the accessory gonads, only careful palpation through the rectum is permissible in order to determine changes in the size, shape and consistency of these organs. However, with torpid, protracted and chronic urethritis, suspicion of damage to the prostate gland, seminal vesicles and bulbourethral glands, it is necessary to obtain their secret for research with the help of massage, since palpation is not always possible to identify pathology.
The prostate gland is palpated in the knee-elbow position of the patient with a slightly arched back. He can also stand facing the table with his knees straight and legs slightly apart and his torso bent at a right angle, resting on his elbows. Patients who for some reason (polyarthritis, etc.) cannot take one of these positions are examined in a side position with knees bent and legs brought to the stomach. However, this position is inconvenient, because due to the inevitable deviation of the central groove from the horizontal line, a false impression of the asymmetry of the organ will be created.The study is best done shortly after urination, because with a full bladder, the prostate gland pushed into the lumen of the rectum may seem enlarged.
The index finger of the right hand in a rubber glove or in a fingertip with a protective circle made of medical oilcloth is smeared with petroleum jelly or another non-irritating fat-like substance (a thick emulsion of neutral soap is convenient, which is then easily washed off with water). A straightened finger is slowly inserted into the rectum, where, at a distance of 4-5 cm from the anus, the lower pole of the prostate gland is felt. Carefully sliding a finger along its surface, assess the clarity of the boundaries, the size, shape, severity of the central groove, the symmetry of the left and right lobes, the appearance of the surface and the consistency of the prostate gland. Pay attention to the presence of infiltrates, nodes, fluctuating foci, depressions, calculi, as well as the localization and severity of pain.
The unaltered prostate resembles in size and shape a small chestnut tree, with its rounded top down. Usually the finger freely reaches the upper border of the non-enlarged prostate gland. Sometimes it has a distinct semilunar notch; according to I.F. Yunda (1974), such a sickle gland occurs with androgen deficiency. However, the sickle-shaped prostate may be due to the presence of a large central dimple at its base (possible enlargement of the utriculus musculinus). This anomaly contributes to the stagnation of secretions in the enlarged utriculus musculinus, which leads to infection of the seminal vesicles.
The surface of the prostate gland, which is felt through the anterior wall of the rectum, is smooth, slightly convex or flat. The central groove divides the gland into two identical lobes, clearly separated from the surrounding tissues. Even in a healthy person, gentle pressure on the prostate causes discomfort that radiates to the penis. With varicose symptom complex, anal fissures, proctitis, pain is localized outside the boundaries of the prostate gland.
Due to the different size, shape and consistency of the prostate gland, for a correct assessment of its condition, these and other features of the left and right lobes should be compared, and the results of the study of the secret should be taken into account. Changes detected during palpation are conveniently documented graphically in the medical history.
To obtain the secret of the prostate gland, its diagnostic massage is performed. Of course, this procedure is contraindicated in acute inflammation of the prostate gland and other accessory gonads, in acute urethritis, orchitis, uroarthritis. Diagnostic massage is performed after urination, and with discharge from the urethra after its preliminary washing with an isotonic sodium chloride solution, which is especially necessary in cases where a bacteriological examination of the secret is expected.
First one, then the other lobe of the prostate gland is massaged with finger movements from the periphery to the central groove along the excretory ducts, trying not to touch the seminal vesicles. Finish the massage by pressing on the area of the central sulcus from top to bottom. The duration of the massage should not exceed 1 minute. The secret released from the urethra is collected in a sterile test tube or on a clean glass slide for research. Sometimes the secret of the prostate from the urethra does not follow. In such cases, the patient is recommended to immediately get on his feet Tiktinsky OL, 1984. If, nevertheless, the secret could not be obtained, this means that he did not get into the urethra, but into the bladder. Then the centrifugate of the washing liquid released from the bladder after prostate massage is examined. Despite washing the urethra, contamination (contamination) of the secretion of the prostate gland with urethral flora inevitably occurs. More accurate results are given by cultures of the secret obtained during transperineal puncture of the prostate gland.
Negative results of a single examination of the secretion do not mean that there are no pathological changes in the prostate gland.
Since the pathologically altered secret becomes much more viscous, and individual excretory ducts can be squeezed by the infiltrate located in the stirrup, the massage will primarily release the secret from the unaffected glands, resulting in a false impression of well-being. For example, M.I. Kaplun (1984) in 23.5% of patients with chronic prostatitis observed a low content of leukocytes in the secretion of the prostate gland due to the focality of pathomorphological changes. Therefore, the study of the secret must be carried out repeatedly.
The composition of the secret objectively reflects the state of the prostate gland, and the study of the secret allows you to identify pathological changes in the gland in cases where no abnormalities are detected during palpation.
In addition to repeated microscopic and bacteriological studies, biochemical analyzes are carried out in some cases, since the normal composition of the secretion indicates the full function of the prostate gland.
Microscopic examination of native preparations in a hanging or crushed drop in a dark or darkened field of view using a diaphragm and a lowered Abbe condenser shows a large number of small (1-2 microns) rounded or angular particles that refract light poorly. These are the so-called lipoid, or lecithin, grains (bodies), which are the product of normal secretion of the glandular epithelium of the prostate gland. In the normal state of the prostate gland, lipoid grains densely cover the entire field of view: 1 ml of secretion in men under the age of 30-40 years contains 5-10 million grains or more. It is the lipoid grains that mainly determine the opalescence of the secretion of the prostate gland. A decrease in their content indicates a decrease in the function of the prostate gland and correlates with the prevalence of its lesion.
Significantly less in the secret of layered (amyloid) bodies, which are stained purple or blue with Lugol's solution, like starch. The size of amyloid bodies is from a few microns to a pinhead and more. In large bodies, their layered structure is clearly visible. The presence of amyloid bodies in secret is an indicator of good prostate function.
According to the results of microscopy of the prostate secretion, the diagnosis of prostatitis is established when the number of polymorphonuclear leukocytes>10 in the field of view of a light microscope (280 times magnification) Madsen P.O. et al., 1994, although, according to E.M. Meares (1990), the presence of prostatitis is indicated by an increase in the number of leukocytes up to 15 in the field of view. The most objectively about inflammation in the prostate gland can be judged by counting leukocytes in its secret in a counting chamber. The normal content of leukocytes is considered to be up to 300 cells in 1 μl (300-106 / l). In the absence of leukocytes in the secretion of the prostate gland and the presence of palpation or other signs of chronic prostatitis, it is advisable to carry out a provocation with pyrogenal (prodigiosan), massage of the gland, and diadynamic currents.
In order to diagnose chronic prostatitis, E.M. Meares and T.A. Stamey (1986) proposed a four-glass test based on a comparative bacteriological evaluation of approximately equal portions of urine obtained before and after prostate massage, as well as its secretion. The diagnosis of prostatitis is established when the concentration of microbes in the third portion of urine is ten times higher than in the first portion.
The following concentrations of microorganisms (CFU / ml) according to W. Weidner, 1984 can indicate the diagnosis of prostatitis:
- the first portion of urine (10-15 ml) 104; - the third portion of urine (after massage) (10-15 ml) >103.
In the secret that is obtained after massage, single (or in a small amount) cells are found from the superficial, intermediate or basal layer of the epithelium of the excretory ducts of the prostate gland. The cells of the superficial layer are rather large, polygonal, with a very small pycnotic nucleus and homogeneous chromatin. The cells of the intermediate layer are much smaller, have a cubic or round shape, contain a larger nucleus and chromatin of a pronounced structure. The cells of the basal layer are even smaller, round in shape, with a rather large nucleus. If the secret is obtained by aspiration biopsy, then the cells of the glandular epithelium in it are of the same size, oval in shape, with a uniformly stained cytoplasm and a rounded nucleus in the center
See chapter 1 for the composition of prostate secretion
A valuable diagnostic test indicating inflammation of the prostate gland is the phenomenon of crystallization of its secret. This test is actually based on the dependence of the shape of precipitated sodium chloride crystals on the physicochemical properties of the prostate secretion. We found that crystallization disorders were observed in most patients with chronic prostatitis (even without sexual disorders), and the degree and frequency of these disorders were directly related to the intensity the duration of the inflammatory process in the prostate
Methodology A drop of prostate secretion is applied to a defatted clean glass slide and dried at room temperature. Then, a drop of isotonic sodium chloride solution of the same size is layered on it, dried in air at room temperature and microscoped. During normal crystallization, a peculiar pattern is visible that resembles a fern leaf. When the prostate gland is affected, various deviations from this picture are noted.
For the purpose of early detection of chronic prostatitis, we also use the determination of the antioxidant activity (AOA) of prostate secretion, which in healthy donors ranges from 74.48 to 88.76%. 5 (31.25%) of 16 people, and in the group of patients in 19 (79.17%) of 24 (p) are not palpable. In addition, sometimes it is not possible to insert the index finger to the required depth even in cases where the filled bladder somewhat pushes the high-lying seminal vesicles down and creates a relative support that facilitates their detection in the loose paravesical tissue. BA Teokharov (1968) recommends conducting a bimanual palpation with an empty bladder in this way he succeeded in 67% of healthy men to probe - one or both seminal vesicles in the form of elongated formations of doughy consistency, located above and lateral to the prostate gland. He emphasizes that normal vesicles are easier to find if they are filled with contents (if the patient has not ejaculated for several days), and the abdominal wall is thin. According to this technique, the seminal vesicles are palpated bimanually between the index finger of the right hand, inserted into the rectum, and the fingers of the left hand, pressing the anterior abdominal wall in the corresponding iliac region.
The Picker method is more often used: the patient, standing on a raised platform (chair, stool) with legs half-bent at the knees and the body tilted forward, as if squatting on the index finger of the doctor’s right hand, leaning his elbow on his right knee, and with his left hand pressing on the lower abdomen of the patient. G.G. Korik (1975) somewhat modified this method: the patient kneels on the couch, slightly tilts the torso forward and sits on the doctor's finger inserted into the rectum.
With catarrhal inflammation of the seminal vesicle, the data obtained by palpation are normal, and the diagnosis can only be established on the basis of the results of a microscopic examination of the secret. In other forms of lesions, soft or dense, compact or fluctuating swellings of various shapes are felt in the area of the seminal vesicles, slightly sensitive or very painful.
In order to obtain the contents of the seminal vesicles in a pure form for research, the prostate gland is first massaged with a full bladder. After urination, during which the secret of the prostate gland squeezed into it and the discharge of the urethra itself are washed out of the urethra, the urethra and bladder are washed with an isotonic solution of sodium chloride, leaving 150-200 ml of liquid in it. Then alternately massage the seminal vesicles for 1 1.5 minutes each, trying not to affect the prostate gland. Massage begins with stroking the distal part of the seminal vesicle (cervix) adjacent to the prostate gland, where the vas deferens is located, gradually increasing the pressure of the finger. Only after that they proceed to massage the upper part (body and bottom) of the bubble with rotational movements of the fingertip up and out. Finish the massage by performing two or three pressing movements from top to bottom to the prostate gland. You can not start the massage from the upper, proximal part, as the thick, viscous secret of the seminal vesicle can clog the vas deferens.
The need for a separate study of the seminal vesicles arises if no changes are found in them during palpation, while an increased content of leukocytes is found in the secret (over 10 in the field of view at a magnification of 280 times). In order to clarify the localization of the lesion, one seminal vesicle is first massaged and its contents are obtained for examination. Then, after urination, the urethra is washed again, the bladder is filled with an isotonic solution of sodium chloride, the second seminal vesicle is massaged, and its contents are sent for examination. With a small amount of content in the seminal vesicle, its secret, spreading over the entire surface of the urethra, may not reach the external opening or stand out in a small amount. In such cases, in order to obtain a secret, and especially if it is necessary to conduct a bacteriological examination, G.G. Korik (1975) proposed to pre-install a catheter with an olive-shaped tip and a syringe that creates a slight vacuum in the posterior urethra.
Microscopic examination of normal contents reveals mobile and immobile spermatozoa, fibrin-like fibers, single polynuclear neutrophils (less than 5 per field of view), sometimes one or two erythrocytes and sympexia (Trousseau-Lallemand bodies) of various shapes, somewhat resembling waxy cylinders.These sympexies give a positive reaction to mucin and dissolve easily in acetic acid.
Leukocytosis in combination with an increased number of red blood cells usually indicates inflammation of the seminal vesicle.
The bulbourethral glands are examined with the patient in the supine position with knees bent and legs apart, pressed against the stomach. The index finger of the right hand is inserted behind the sphincter of the rectum and bent, and the thumb of the same hand is pressed against the perineum near the anus. Palpate the tissue of the perineum below the prostate, trying to find the bulbourethral glands. Normally, these glands are not palpable, but with inflammation they can be found in the form of painful compacted nodes on the side of the midline of the perineum and, with the help of massage, squeeze their secret into the urethra. The urethra and bladder should be flushed first, especially if there is pyuria or urethral discharge. A little isotonic sodium chloride solution is left in the bladder. After massaging the bulbo-urethral glands, the patient releases the washing liquid into a test tube, which is sent to the laboratory for microscopic and bacteriological examination of the centrifugate.
Injury to the prostate and seminal vesicles
The prostate (prostata) is an unpaired organ of the male reproductive system, located in the anterior lower part of the small pelvis under the bladder. Seminal vesicles (glandula seminalis) are paired formations related to the internal male genital organs and protruding as part of the vas deferens.
The prostate and seminal vesicles are located in the depths of the small pelvis, protected by its bones and muscular-aponeurotic formations of the perineum; anatomically and topographically closely related to the bladder, urethra (urethra), rectum, urogenital diaphragm, so their damage is most often multiple and combined.
Closed and open injuries of the prostate and seminal vesicles are distinguished. Depending on the type of injury, bruises and lacerations are distinguished among closed injuries, with open injuries - bruises, tangential, blind and through wounds.
Closed lesions of the prostate and seminal vesicles
Closed damage to the prostate and seminal vesicles can occur with fractures of the pelvic bones, a strong blow to the perineum or a fall on it. Bruises and ruptures of these organs are usually combined with damage to the venous plexus adjacent to them. At the same time, the membranous and prostatic parts of the urethra and the rectum can be damaged.
Iatrogenic damage to the prostate also occurs with the forced introduction of metal instruments into the posterior urethra, especially when it narrows (urethral stricture) or prostate adenoma.
Endourethral damage to the prostate can be single or multiple and are called false passages. There are an incomplete false passage (they do not penetrate the entire prostate) and a complete false passage (penetrating beyond it into the pelvic tissue, seminal vesicles, bladder, rectum).
Symptoms of closed injuries of the prostate and seminal vesicles:
- Pain in the anus and perineum.
- Difficulty with painful urination.
- Hematuria.
- Hemospermia.
In severe trauma, combined with significant damage to the pelvic bones, clearly expressed symptoms of the latter smooth out or hide the clinical manifestations of damage to the prostate and seminal vesicles. Injury (damage) to the seminal vesicles in all cases are recognized late, as they do not have specific symptoms.
Endourethral injuries of the prostate are manifested by pain in the perineum, bleeding from the urethra (urethra), painful difficulty urinating, acute urinary retention (AUR).
Combined injuries of the prostate and urethra or bladder, complete false passages can lead to urinary leakage, urinary infiltration and the occurrence of phlegmon of the pelvic tissue. In some cases, urosepsis develops.
The diagnosis is established on the basis of anamnesis, assessment of existing symptoms, examination results.
At rectal examination, the prostate is enlarged in size, uneven consistency: it may show areas of softening, infiltration of paraprostatic tissues due to hemorrhage or urohematoma is determined. Her palpation is sharply painful.
Ultrasound (ultrasound diagnostics) and CT (computer diagnostics) are of great help in diagnosing damage to this localization. On urethrocystograms, leakage of the contrast agent into the prostate, paraprostatic tissue can be seen.
For prostate bruises, patients are prescribed bed rest, painkillers, hemostatic and antibacterial drugs. With urinary retention, it is advisable to establish a permanent balloon catheter; sometimes used capillary puncture of the bladder, there may be indications for cystostomy.
To stop bleeding from the prostate, in addition to conventional hemostatic agents, they successfully use a pressure bandage on the perineum, local hypothermia, tamponade of the bleeding prostate and the prostatic part of the urethra with a dosed tension of the balloon-catheter using a fixed aseptic napkin on the urethral catheter at the external opening of the urethra .
With ruptures of the prostate, its injury by fragments of the pelvic bones with extensive hemorrhages, sometimes there is a need for surgical treatment. It consists in exposing the prostate by perineal or retropubic or vesical access, removing bone fragments, outflowing blood and clots from it, stopping bleeding by applying eight-shaped sutures or tamponade of the damaged and bleeding prostate.
Open injuries of the prostate and seminal vesicles
Open injuries of the prostate and seminal vesicles are observed with gunshot and stab wounds. Gunshot wounds (bullet, shrapnel, mine-explosive) of these organs were quite rare during the Great Patriotic War and, as a rule, were combined. In modern military conflicts, mine-explosive wounds, which are always combined, predominate.
Stab wounds occur in domestic, industrial or military conditions when sharp piercing objects are introduced through the perineum or rectum. The same group includes iatrogenic damage to the prostate and seminal vesicles during surgery for removal of the rectum and bladder, prostate biopsy, paraprostatic blockade, etc.
The anatomical location of the prostate in the small pelvis predisposes to combined injuries of the bladder and pelvic bones. In this regard, the clinical signs of prostate injury are smoothed out or hidden by symptoms of damage to the bladder and pelvic bones. Only after some time, continuing hematuria, urination disorders (dysuria) and pain in the perineum and anus, radiating to the head of the penis, make one suspect a prostate injury.
The main symptoms of stab wounds of the prostate are bleeding, pain in the perineum and rectum, radiating to the head of the penis, and dysuria (urination disorders). With combined injuries of the urethra (urethra), bladder and rectum, streaks of urine can join, its excretion through the rectum or perineal wound, fecal discharge and gases through the wound.
The most characteristic sign of open damage to the seminal vesicles is the outflow of sperm from the wound or the formation of fistulas.
The diagnosis of prostate injury is established taking into account the localization of the inlet and outlet openings and the projection of the wound channel, examination of the perineum, digital rectal examination, which makes it possible to determine the deformation of the organ. Often the fact of injury to the prostate is confirmed during surgery for injury to the bladder.
Diagnosis of stab wounds is based on an assessment of complaints, anamnesis, localization of the wound, the projection of the wound channel, the results of a physical examination with mandatory palpation of the prostate, the data of a survey radiograph of the pelvic region, urethro- and fistulograms, ultrasound and CT of the pelvic organs. MRI (magnetic resonance imaging) not only reveals damage to the prostate, but also to surrounding tissues.
Therapeutic tactics for combined injuries of the bladder and prostate is always operational and is determined, first of all, by localization and the need for an emergency stop of bleeding. In other cases, the sequence of actions of the urologist includes performing a lower median laparotomy, primary treatment and suturing of bladder wounds, sanitation and drainage of the abdominal cavity with an intraperitoneal wound of the bladder, sparing treatment of the prostate wound, hemostasis, vesical fistula, drainage of perivesical and paraprostatic tissue, suturing of a laparotomic wound , treatment and drainage of musculoskeletal wounds and immobilization of bone fragments.
Treatment of wounds of the prostate consists in the primary surgical treatment of the wound, removal of foreign bodies, stopping bleeding, opening and draining urinary streaks and abscesses. With simultaneous damage to the urethra (urethra) and rectum, a cystostomy is applied, an unnatural anus (colostomy), the pelvic tissue is drained. In case of damage to the seminal vesicles, it is usually limited to drainage of the wound.
Conservative treatment is possible for mild isolated wounds of the prostate with minor bleeding and no signs of inflammation. An example would be treatment after an uncomplicated prostate biopsy.