Home >
Erectile Dysfunction >
Histology in prostate cancer
Histology in prostate cancer
Gleason's histological classification of prostate cancer.
At present, Gleason's histological classification has found the widest application, as it largely meets the requirements of the clinic when choosing treatment tactics and disease prognosis.
Gleason's classification is based on the degree of differentiation of the glandular structures of the tumor. A tumor according to the Gleason score of 1 is formed by almost normal glands, the structure of which is lost as the Gleason score increases, and with a score of 5, the tumor is characterized by undifferentiated cells. The more tissue differentiation is lost, the worse the prognosis for this patient.
According to the Gleason classification, the degree of tumor differentiation is divided into five gradations:
- gradation 1: the tumor consists of small homogeneous glands with minimal changes in the nuclei;
- gradation 2: the tumor consists of clumps of glands, still separated by the stroma, but closer together;
- gradation 3: the tumor consists of glands of various sizes and structures and, as a rule, infiltrates the stroma and surrounding tissues;
- gradation 4: the tumor consists of clearly atypical cells and infiltrates the surrounding tissues;
- gradation 5: the tumor consists of layers of undifferentiated atypical cells.
With rare exceptions, Prostate Cancer has a heterogeneous structure. Therefore, in order to calculate the Gleason score, the two most common gradations are summed up. For example, examination reveals that the most common tumor is composed of atypical cells and infiltrates surrounding tissues, corresponding to grade 4. In addition, a tumor consisting of a collection of glands, still separated by the stroma, but located closer to each other, is also often found. different, which corresponds to gradation 2. In this case, other variants of the structure of tumors can occur, but only the indicators of the two gradations with the largest value (in our example 4 + 2), i.e. the Gleason score is 6. The resulting score serves as an important prognostic criterion, suggesting faster disease progression, metastasis, and reduced survival.
An analysis of the outcomes of expectant management in the treatment of Prostate cancer showed that in patients with a Gleason score of less than 4, the tumor metastasized in 2.1% of cases per year, in patients with a Gleason score of 5 to 7 in 5.4% of cases, and in patients with a Gleason score of less than 4 Gleason more than 7 in 13.5% of cases.
After the patient has established and morphologically confirmed the presence of prostate cancer, the question arises of establishing the stage of the disease. Accurate knowledge of the stage of the tumor process is a prerequisite for making a decision about the possibility and necessity of performing a radical prostatectomy for a particular patient. According to the concepts prevailing in modern oncourology, surgical treatment is not indicated for patients with metastatic lesions. In addition, the ideal candidate for radical prostatectomy has a tumor that does not extend beyond the periprostatic capsule. However, it is widely known that 50% of patients with a palpable T2 prostate tumor have only histologically detectable signs of extracapsular invasion. Among patients with stage T1, this figure approaches 25%. From this, the need to improve the preoperative examination of patients with suspected prostate cancer is obvious.
Histology in prostate cancer
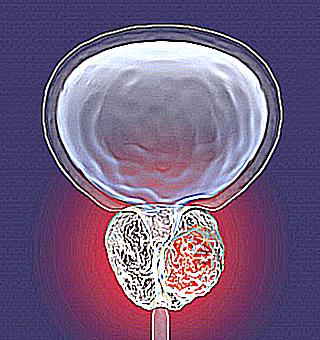
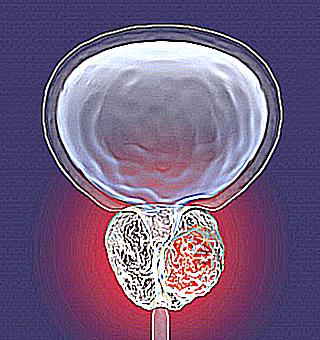
Prostate cancer is a malignant neoplasm arising from the epithelium of the alveolar cell ducts of the prostate.
In all developed countries of the world, prostate cancer is the leading oncological disease in men. At the same time, prostate cancer is one of the most common causes of death in older men, for example, in the United States, prostate cancer is the third most common cause of death from malignant tumors.
Histological classification of prostate cancer
At histological examination, the following forms of prostate cancer are distinguished:
- Polymorphic cell carcinoma (a large number of dividing cells of various shapes and sizes)
- Anaplastic adenocarcinoma (changes in intracellular structures, characteristic shape and size of cells)
- Solid cancer (cells are arranged in layers or strands separated by layers of connective tissue)
- Scirrhous cancer (the tumor becomes solid, fibrous due to the predominance of connective tissue stroma over tumor cells)
- Adenocarcinoma (if cancer originates from glandular epithelium)
- Squamous (if the cancer originated from squamous epithelium)
- Tubular (appearance from narrow channels lined with epithelium, in the lumen of which there may be a secret)
- Cubic tubular carcinoma
- Prismatic tubular carcinoma
- Alveolar (arises from the terminal divisions of branching glands)
There are precancerous conditions, the timely detection of which helps to prevent cancer.
These include:
- Atypical prostatic hyperplasia (facultative precancer of the prostate that can develop into prostate cancer under certain conditions)
- Intraepithelial neoplasia of the prostate (obligate precancer of the prostate, precursor to adenocarcinoma of the prostate).
Causes of prostate cancer
A number of factors have been identified that affect the appearance and development of prostate cancer. This is:
TNM classification of prostate cancer
This classification was developed by the International Cancer Union. With its help, the prevalence of the tumor in the gland and the human body is determined. The letters TNM are an abbreviation of the Latin words Tumor (tumor), Nodulus (node - in this case, we mean the lymph nodes), Metastasis (metastases). The combination of TNM values determines the stage of prostate cancer (from one to four).
T primary tumor. TX is insufficient data to assess the primary tumor. T0 primary tumor is not determined. T1 tumor is not clinically manifested, is not palpated and is not visualized by special methods. T1a tumor is incidentally detected during histological examination and makes up less than 5% of the resected tissue. The T1b tumor is found incidentally on histological examination and accounts for more than 5% of the resected tissue. A T1c tumor is diagnosed with a needle biopsy (performed due to a high PSA level). T2 tumor limited to the prostate or extending into the capsule. T2a tumor involves half of one lobe or less. T2b tumor involves more than half of one lobe, but not both lobes. T2c tumor affects both lobes. T3 tumor extends beyond the prostate capsule. T3a tumor extends beyond the capsule (unilateral or bilateral). T3b tumor extends to the seminal vesicle. T4 non-displaceable tumor or tumor that invades adjacent structures (but not seminal vesicles): bladder neck, external sphincter, rectum, levator ani, and/or pelvic wall.
N regional lymph nodes. The regional lymph nodes for the prostate are the pelvic lymph nodes located below the bifurcation of the common iliac arteries. Category N does not depend on the side of localization of regional metastases. NX insufficient data to evaluate regional lymph nodes. N0 metastases in regional lymph nodes are absent. N1 there are metastases in regional lymph nodes.
M distant metastases. MX to determine the presence of distant metastases is not possible. M0 signs of distant metastases are absent. M1 distant metastases. M1a involvement of non-regional lymph nodes. M1b bone lesion. M1c other sites of distant metastases.
Prostate Cancer Clinic
Many of the symptoms of prostate cancer, especially in the early stages, are similar to those of benign prostatic hyperplasia. These include the so-called:
In the case of advanced prostate cancer with the development of metastases, pain in the bones, above the womb, in the perineum may occur. It must be taken into account that metastases spread hematogenously and along the lymphatic tract.
Bone metastases are most common, especially in the pelvis. Metastases to the lymph nodes are often not combined with metastasis to the bone tissue.
Diagnosis of prostate cancer
Based on the sequence of execution, the following methods for diagnosing prostate cancer are used:
- Magnetic resonance imaging of the pelvic organs
- radioisotope studies of the skeleton
- X-ray examinations of bones
- computed tomography
- uroflowmetry
Prostate cancer treatment
Depending on the stage of the process, treatment approaches for prostate cancer differ.
For local forms (T1-2N0M0, without metastases) of prostate cancer, the main methods of treatment are:
- open or laparoscopic radical prostatectomy, in which the prostate is removed en bloc with seminal vesicles, and lymphadenectomy is also performed. According to indications, nerve-sparing prostatectomy is performed in order to maintain an erection.
International histological classification of prostate cancer.
Adenocarcinoma (small acinar, large acinar, cribriform, solid or trabecular and others).
Cancer of the glandular structure (adenocarcinoma) is the most common. It accounts for 90% of all malignant epithelial tumors of the prostate.
Morphological verification of a prostate tumor must necessarily include determining the degree of differentiation, in other words, the degree of malignancy of the tumor.
G1 - high degree of differentiation;
G2 - moderate degree of differentiation;
G3-4 - low degree of differentiation or no differentiation.
Gleason's (1977) morphological grade system is currently considered the most acceptable. The Gleason system offers five variants of adenocarcinoma histostructure - from the most mature acinar (type 1) to completely undifferentiated solid (type 5). Assessment of the degree of malignancy (Gleason score) is carried out by arithmetic addition of the two most common structural variants in the material under study. The total indicator (Gleason score) is evaluated on a scale of 2-10 and is considered an important prognostic sign; so, for example, with an indicator of 8 or more, the probability of metastatic lesions and tumor germination beyond the prostate capsule is high.
Correspondence between the Gleason sum indicator and the degree of adenocarcinoma differentiation (G):
Gleason score 2-4 - G1;
Gleason score 5-6 - G2;
Gleason score 7-10 - G3-4.
TNM classification
Classification of the International Cancer Union according to the TNM system (2009).
The TNM classification below applies only to adenocarcinoma. Transitional cell carcinoma of the prostate is classified as a tumor of the urethra.
T - primary tumor.
TX - not enough data to evaluate the primary tumor.
T0 - the primary tumor is not detected.
T1 - the tumor is not clinically manifested, is not palpable and is not visualized by special methods.
T1a - the tumor is incidentally detected during histological examination and makes up less than 5% of the resected tissue.
T1b - the tumor is incidentally detected during histological examination and makes up more than 5% of the resected tissue.
T1c - the tumor is diagnosed with a needle biopsy (performed due to a high level of prostate-specific antigen).
T2 - the tumor is limited to the prostate gland or extends into the capsule (but not beyond).
T2a - the tumor affects half of one lobe or less.
T2b - the tumor affects more than half of one lobe, but not both lobes.
T2c - the tumor affects both lobes.
Note. Tumor diagnosed by needle biopsy in one or both lobes, but not palpable and not visualized, is classified as T1c.
T3 - the tumor spreads beyond the capsule of the prostate gland.
T3a - Tumor extends beyond the capsule (unilateral or bilateral), including microscopic extension to the bladder neck.
T3b - the tumor spreads to the seminal vesicle (or both vesicles).
Note. Tumor extension to the apex of the prostate or into the capsule (but not beyond) of the prostate is classified as T2, not T3.
T4 is a non-displaceable tumor or a tumor that has spread to adjacent structures (other than seminal vesicles): external sphincter, rectum, levator ani, and/or pelvic wall.
N - regional lymph nodes.
The regional lymph nodes for the prostate are the pelvic lymph nodes located below the bifurcation of the common iliac arteries. Category N does not depend on the side of localization of regional metastases.
NX - insufficient data to evaluate regional lymph nodes.
N0 - no metastases in regional lymph nodes.
N1 - there are metastases in regional lymph nodes.
Note. Metastases no larger than 0.2 cm should be referred to as pN1mi.
M - distant metastases.
MX - it is not possible to determine the presence of distant metastases.
M0 - there are no signs of distant metastases.
M1 - distant metastases.
M1a - defeat of non-regional lymph nodes.
M1b - bone lesion.
M1c - other sites of distant metastases.
Depending on the combination of criteria T, N, M and G, the stage of the disease is determined: