Home >
Erectile Dysfunction >
Standard for the treatment of prostatitis in a hospital
Standard for the treatment of prostatitis in a hospital
Russian doctor
Login with uID
Articles catalog
Modern methods of prostatitis treatmentStandards for the treatment of prostatitis Protocols for the treatment of prostatitis
Inflammatory diseases of the prostate
Profile: surgical Stage: hospital Stage goal: reduction of symptoms and elimination of infection with minimal adverse effects, restoration of copulative and fertile functions Duration of treatment (days): 12
ICD codes: N41.1 Chronic prostatitis
Definition: Chronic prostatitis is an inflammation of the prostate gland of infectious and congestive origin.
Classification (National Institute of Health, USA): Chronic bacterial prostatitis Chronic bacterial prostatitis (chronic pelvic pain syndrome) type A with an increase in the number of leukocytes in the secretion of the prostate type B without an increase in the number of leukocytes in the secretion of the prostate Asymptomatic inflammation of the prostate gland Catarrhal, follicular .
Risk factors: sexually transmitted diseases, hormonal disorders, impotence and infertility.
Indications for hospitalization: Pain in the perineum, dysuria, complications (copulative, fertile dysfunction and failure of outpatient treatment).
Required volume of examinations before planned hospitalization: OAM, microreaction, fluorography, prostate secretion, urine portion after prostate massage, 2-glass sample, bacteriological examination of urine after massage, PSAg concentration, PCR, ELISA, RIF, PIF, spermogram , research on hormones.
Diagnostic criteria: 1. Increased urination, burning sensation in the lower abdomen. 2. Difficulty in urination, painful urination. 3. Feeling of incomplete emptying of the bladder. 4. Feeling of pressure in the perineum, anus and anterior to it. 5. Pain in the testicles or glans penis. 6. Hematospermia, painful ejaculation, accelerated ejaculation. 7. Decreased libido, partial erectile impotence with a long course. 8. Fever and deterioration in general well-being. 9. Soreness on palpation of the lower abdomen. 10. Severe tenderness of the prostate gland on palpation. 11. A large number of leukocytes, mucus and bacteria in the urine. 12. Ultrasound: a picture of chronic prostatitis.
The list of the main diagnostic measures: 1. Complete blood count (6 parameters) 2. Complete urinalysis 3. Sowing of biological fluid with the selection of colonies 4. Analysis of the sensitivity of microbes to antibiotics 5. Ultrasound of the bladder
List of additional diagnostic measures: 1. ELISA Chlamianitigen 2. ELISA chlamydia IgA 3. ELISA ureaplasmosis IgM 4. ELISA trichomoniasis IgG 5. ELISA herpes IgM 6. ELISA gardnerellosis 7. ELISA cytomegalovirus 8. Test for fungi of the genus Candida with the study of morphology 9. ELISA mycoplasmosis
Treatment tactics: 1. Elimination of the etiological factor (antibiotic therapy according to the sensitivity of the microbial flora) fluoroquinolones (norfloxacin 400 mg 2 times a day, ciprofloxacin 250-500 mg 2 times a day), cephalosporins 2.3 generation (effective ceftriaxone 1 0 g 1 time / day / m 7-10 days), amoxicillin + clavulanic acid and clindamycin, macrolides (clarithromycin, sumamed, azivok, roxithromycin), tetracyclines, etc.
2. For the treatment and prevention of mycosis during prolonged massive antibiotic therapy, itraconazole oral solution 400 mg daily for 7 days.3. b-blockers (tamsulosin, terazosin 1-2 or 2.5 times a day or alfuzosin 2.5 mg 1-2 times a day) in combination with antibacterial drugs). 4. Organotropic preparations (prostacor, vitaprost suppositories).5. Prostate massage, sitz baths, biofeedback methods (pelvic floor muscle training). 5. Immunotherapy (timogen, cycloferon).
Chronic non-bacterial prostatitis. Efficacy not established: b-blockers, 5a-reductase inhibitors, anti-inflammatory drugs (pentosan polysulfate sodium), transurethral microwave thermotherapy, allopurinol.
If there is a violation of the relaxation of the sphincter of the bladder and / or the neck of the bladder, a transurethral incision of the bladder neck is indicated.
List of essential medicines: 1. Gentamicin injection 40 mg / ml, 80 mg / 2 ml in an ampoule 2. Cefuroxime 250 mg, 500 mg tab; powder for the preparation of an injection solution in a vial 750 mg 3. Itraconazole oral solution 150 ml - 10 mg ml 4. Nitroxoline 200 mg tab 5. Ketoprofen rectal suppositories 6. Metronidazole solution for infusion in a vial, 250 mg tab 7. Ampicillin tablet 250 mg; capsule 250 mg, 500 mg; powder for injection solution 500 mg, 1000 mg; suspension 125/5 ml in bottle
List of additional medicines: 1. Acyclovir 200 mg tab.; powder in a vial 205 mg 2. Liquid aloe vera extract 1 ml amp 3.Levofloxacin 250 mg, 500 mg tab
Criteria for transfer to the next stage: No complaints about the clinical manifestations of the disease, improvement in well-being, normalization of indicators of control tests of prostate secretion, ELISA.
N 1673n On approval of the standard of primary health care for chronic prostatitis (examination for diagnosis and treatment)
N 1673n On approval of the standard of primary health care for chronic prostatitis (examination for diagnosis and treatment)
See help about standards of care
In accordance with Article 37 of the Federal Law of November 21, 2011 6724; 2012, N 26, Art. 3442, 3446) order:
Approve the standard of primary health care for chronic prostatitis (examination for diagnosis and treatment) according to the annex.
Registration N 27484
A standard of medical care has been approved that defines the basic requirements for the diagnosis and treatment of patients with chronic prostatitis (examination for diagnosis and treatment). The standard is recommended for use in the provision of primary health care.
N 1673n On approval of the standard of primary health care for chronic prostatitis (examination for diagnosis and treatment)
Registration N 27484
This order comes into force 10 days after the date of its official publication
N 134/1 (special edition)
Standard for the treatment of chronic prostatitis
Have you been struggling unsuccessfully with PROSTATITIS and POTENTITY for many years?
Head of the Institute: "You'll be amazed at how easy prostatitis can be cured by taking it every day.
Our readers have successfully used M-16 to improve potency. Seeing the popularity of this tool, we decided to bring it to your attention. Read more here-
Prostatitis is an inflammatory and degenerative lesion of the prostate gland (in some cases it is dystrophic, in others it is inflammatory, but it can also be of mixed origin). The disease affects mainly older men: men over 40 years of age are at risk. Unfortunately, in recent years, the disease has acquired a tendency to rejuvenate, so we can say that both young people and older people suffer from it equally.
Prostatitis is dangerous with a high probability of violations of the reproductive system: it is possible to develop low sperm motility and, as a result, relative infertility, which is difficult to treat. What do you need to know about this disease if you want to maintain male sexual health?
Brief anatomical information about the prostate
The prostate gland is an exocrine (releasing substances outside the body) gland of the muscular-glandular structure. The localization of the organ is the area of the bladder. The prostate (another name for the prostate gland) performs several important reproductive functions:
There are also less significant functions of this male organ (read more about the structure and function of the prostate here).
What is prostatitis: definition of the disease
In urology, prostatitis is understood as a lesion of the prostate gland of various origins: it can be either directly inflammation or a non-inflammatory process that entails degeneration of this organ. Depending on the etiology of the disease, the appropriate treatment is selected, therefore it is so important not to engage in self-therapy, but at the first "malfunctions" with the genitourinary system, go to the doctor.
Etiology/pathogenesis of prostatitis
Etiology and pathogenesis (the origin and mechanism of the formation of the disease) is one of the most controversial issues in modern urology. In domestic science and practice, there is a strong opinion that prostatitis is an inflammatory lesion of the prostate gland of an infectious origin. But this is true only in part and not always. It is about her that they usually talk about prostatitis. But not everything is so simple and obvious.
Prostatitis may not be accompanied by inflammation at all. In this case, they speak of a non-inflammatory form of the disease. The non-bacterial form of prostatitis accounts for about the remaining 90% of cases of pathology. A contextual synonym for prostate damage of non-inflammatory and non-infectious origin in European medical practice is the name "chronic pelvic pain syndrome".
According to the most advanced scientific views, the etiology of prostatitis is complex: the organ comes into complete hormonal, hematological and physical dissonance. Both muscles and glandular cells cease to function normally. We are talking about the multifactorial origin of the disease.
There are three main theories about the etiology of prostatitis:
- Theory 1.The first states that the basis for the development of the disease is an acute viral/infectious disease. This, as it has already turned out, is far from always true.
- Theory 2. The second one speaks of the vascular origin of the imbalance. We are talking about ischemia of the prostate. As a result of one or another factor, the development of insufficiency of the blood supply to the organ occurs. As a result, it completely or partially loses its functions: after all, nutrition and oxygen saturation in a normal amount are absent. Read on the topic: Treatment of blood stasis in the pelvis.
- Theory 3. The third theory presents a picture of the pathology of the prostate gland as a neurogenic disease. According to this approach, there are no organic causes of morbidity, we are talking about neurogenic pain.
Thus, both etiology and pathogenesis are multifactorial.
Causes for the development of pathology (factors of pathogenesis)
Prostatitis is a polyetiological disease. In practice, this means that it can be caused by a variety of reasons. Among them:
Lack of physical activity (physical inactivity). Movement, as you know, is life. In the absence of rational physical activity, congestion occurs in the pelvic organs. As a result, dystrophy of the glandular organ develops. Obesity. Large body weight indirectly affects the development of prostatitis. We are talking about the same stagnant processes. In addition, as you know, obesity is formed with malnutrition, or metabolic disorders (lipid metabolism). Metabolic disorders cause atherosclerosis. The vessels of the body, including the prostate, are exposed to the deposition of cholesterol. As a result, blood circulation in the pelvic organs changes significantly. Eating a large amount of spices, seasonings. Spicy food irritates the prostate. Irregular sex life. Irregular sexual contacts lead to stagnation of the secret in the structure of the prostate. Stagnation entails an inflammatory process and, as a result, the described disease is formed. Read on the topic: Male sexual abstinence - when is it good and when is it harmful? Disorders of the pelvic organs, primarily the intestines. Crohn's disease, colitis, hemorrhoids. All these diseases lead to insufficiency of venous circulation. Blood cannot circulate normally, as a result, congestion develops in the genitals (pelvic organs).
Hypothermia. Hypothermia causes inflammation in the structure of the prostate. As a rule, this happens due to a decrease in immunity and the activation of pathogenic microflora. Alcohol abuse, smoking. Alcohol, like tobacco, causes stenosis (narrowing) of the lumen of large vessels that feed the prostate gland. The result is already known. The presence of an infectious agent in the structure of the prostate. He can get there from a variety of sources. So, any focus of chronic infectious inflammation can lead to damage to the prostate (for more details: How to recognize hidden sexual infections?). Hormonal disorders. Changes in the hormonal background can cause problems with blood microcirculation, due to excessive effects on the receptors of prostate cells. Arterial hypertension. Insulin resistance. Vitamin deficiency (avitaminosis) (see Vitamins for Prostate Health). Bladder emptying frequency disorders. If a man does not visit the toilet often enough, the pathological flora can penetrate from the bladder into the prostate, causing a septic lesion of this important organ. Lack of muscle work. Promotes insufficient contraction of the muscles of the prostate gland. As a result, the secret of the organ is not sufficiently ejected. Classification of prostatitis There are two bases for the classification of prostatitis. The first reason is the form of percolation. The second is the initial cause of the development of the disease.
Due to the formation of pathology, prostatitis is divided into:
Our readers have successfully used M-16 to improve potency. Seeing the popularity of this tool, we decided to bring it to your attention. Read more here-
- Bacterial prostatitis. Caused by pathogenic microorganisms.
- Viral prostatitis. Its basis is not a bacterium, but a virus. The main difference between a bacterium and a virus is the absence of its own cellular apparatus.
- Neurogenic. According to research data, non-inflammatory neurogenic prostatitis is common. It is caused by violations of the innervation of the gland or by psychogenic causes (a close "relative" of neurogenic pain is the so-called phantom pain).
- Fungal prostatitis.
- Defeat of an organ of a calculous nature (in the presence of stones in the cavity of the gland).
- Herpetic prostatitis. Can be separated into a separate group. Caused by the herpes virus.
Acute and chronic prostatitis are distinguished according to the form of leakage:
- Acute prostatitis occurs with pronounced symptoms, when the clinical picture manifests itself to the greatest extent. The duration of this form is about 6-18 weeks, after which (with proper treatment) the damage to the prostate gland disappears.
- The chronic form develops with untimely treatment. Also, non-infectious prostatitis has a tendency to become chronic (it can already begin with a chronic process).
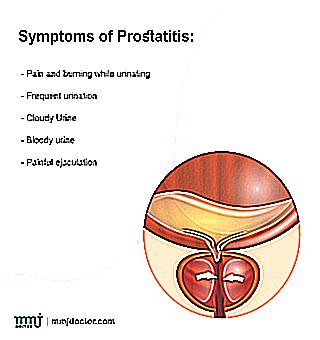
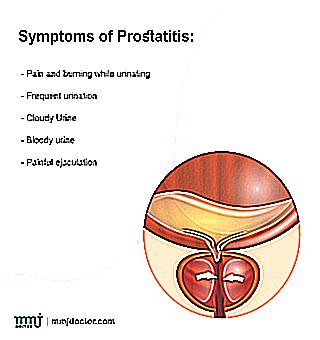
Clinical picture (symptoms)
Acute prostatitis of any origin has characteristic symptoms of two groups: general and focal (local).
General symptoms
Among the common manifestations:
Rise in body temperature to febrile or subfebrile figures (37.5-39 degrees Celsius); headache; general malaise; weakness; drowsiness; feeling of "waddling" of the body. Local symptoms Local symptoms include:
- Pain syndrome in the groin area. Pain is localized in the perineum, given to the scrotum, testicles, penis. The intensity of the syndrome is different: it varies from a weak aching sensation to unbearable pain of a cutting, pulling nature. The strength of the pain increases at the time of urination, intercourse, defecation.
- Missing disorders. The jet becomes weak (due to the proliferation of prostate tissue acting as a valve). Perhaps the complete disappearance of urination.
- Frequent false urge to urinate due to irritation of the walls of the bladder.
- Feeling of incomplete emptying of the bladder.
- Sexual dysfunction (erectile dysfunction) (see How much does prostatitis affect potency?).
- Decreased libido.
The chronic form of the disease is characterized by a complete absence of general symptoms, local signs are observed in an incomplete way: usually we can talk about 2-3 symptoms. In some cases, the clinical picture may be completely absent.
Prostatitis is often a secondary pathology of the genitourinary system. In this case, manifestations of the primary disease (nephritis, pyelonephritis, cystitis, etc.) are mixed with local symptoms.
Diagnosis
Diagnosis begins with a visit to a specialized specialist. The examination does not present any major difficulties. The doctor you should visit is a urologist or urologist-andrologist.
At the initial examination, the doctor asks the patient for complaints, their duration, nature. The duration of the course is extremely important: true prostatitis lasts at least three months, otherwise a revision of the primary diagnosis is required. After the survey comes the turn of a digital examination of the prostate (through the anus). This technique allows the doctor to assess the size and structure of the prostate gland.
The following instrumental and laboratory methods are recognized as the gold standard for diagnosis:
- X-ray of the prostate. It is carried out through the rectum using a special probe. Allows you to assess the size of the prostate, the structure of the organ, the presence of stones.
- Ultrasound examination of the prostate. Required for the same purposes. The most informative among ultrasound examinations of the prostate is TRUS.
- Complete blood count. With an infectious origin of the disease or an inflammatory process, a characteristic clinical picture is revealed with leukocytosis, a high level of ESR (ROE), etc. Erythrocytes, on the contrary, are observed less than normal. Hemoglobin is normal. Specific figures depend on the reference (normal) values adopted by a particular clinic.
- Prostate secretion analysis for bacteria (bacterial cultures). The normal amount of an infectious agent in prostate secretion is 10,000 pathogenic units. Anything more is pathology. So, in this case we are talking about a classic infectious prostatitis. Bacteria, leukocytes in the prostate juice can also be detected. The accuracy of this technique is high. Details of the analysis of the secret of the prostate, see here.
In the complex of these diagnostic methods, it is enough to make a diagnosis.
The basis of treatment is drug (conservative) therapy. Surgical treatment is resorted to only in extreme cases.
Drug therapy
It is based on the following preparations:
Alpha-blockers. According to European studies, they have a pronounced effectiveness. These include: alfuzosin, terazosin, tamsulosin, doxazosin. In some cases, these drugs are unable to reduce pain, so their appointment in combination with analgesics is required. For monotherapy, they are not always suitable. Antibacterial drugs. They are antibiotics. The duration of treatment is selected individually.Specific names of drugs are determined based on effectiveness, however, the selection is carried out empirically (experimentally), since prostate juice cultures do not allow us to draw a conclusion about the pathogen and its sensitivity to antibiotics. Interesting fact. One study evaluated the performance of three drugs: tetracycline, levofloxacin, ciprofloxacin. There were no significant differences in their efficacy. Greater efficiency was noted with a combination of alpha-blockers and antibacterial drugs. However, the effectiveness of antibiotics has not been fully proven. It may well be that the control group lacked uropathogenic microorganisms (see Treatment of Prostatitis with Antibiotics). 5-alpha reductase inhibitors. Data on the drugs in this group are contradictory. Apparently, these drugs cannot be recommended to everyone. However, the effectiveness of pharmaceuticals of this group in elderly patients has been proven. The first and main remedy is finasteride. neuropathological drugs. This is Pregabalin (an antiepileptic drug). Significantly reduces pathological symptoms. Pentosan polysulfate. Well proven in the treatment of chronic pelvic pain. Muscle relaxants (drugs to relax muscles). At the moment, their effectiveness has not been sufficiently studied. The most effective combination of muscle relaxants with anti-inflammatory drugs and alpha-blockers. Among the names: Baclofen, Diazepam. Botulinum toxin. Little studied in the treatment of prostatitis. Has a moderate effect. Antihistamines. Their effectiveness varies, but, in general, proven. It is important to know the underlying cause of prostatitis in a particular case. Antidepressants. They help with the psychogenic nature of the pain syndrome. Immunosuppressants (Azathioprine). Helps reduce pain and urinary frequency. Anesthetics (with intravesical administration of drugs). Hyaluronic acid. Analgesics. Non-steroidal anti-inflammatory drugs. They have high efficiency. This includes Paracetamol, Ketorolac, etc. Neuromodulators (designed to relieve psychogenic pain). See also: Candles for prostatitis - types, list of drugs
You can take anti-inflammatory drugs and analgesics on your own, up to several days at the minimum dosage. But in no case can you be treated on your own. It is strictly necessary to consult a urologist. It is impossible to solve this problem without a doctor. Is it worth risking reproductive health for the sake of a few hours saved?
Surgical treatment is indicated for severe disease. The essence and nature of the operation are determined by the doctor.
Phytotherapy (treatment with folk remedies)
Independent use of phytotherapeutic preparations is acceptable. Cernilton, preparations based on quercetin have the highest proven effectiveness. More controversial efficacy was noted in the extract of serenoa (Serenoa repens). In all cases, pain and the severity of other symptoms decreased.
Prostatitis prevention
It is enough to follow simple recommendations.
You need to have a regular sex life (see Is it possible to have sex with prostatitis?); it is important to adhere to the optimal mode of physical activity and keep the weight at a normal level; it is necessary to abandon the excess of spicy and fatty foods; of great importance in the prevention is the rehabilitation of foci of infectious inflammation, whether it be carious teeth or E. coli; bad habits should be abandoned: smoking, alcohol abuse, etc.; can not be supercooled; it is necessary to treat in time all diseases that can become a source of damage to the prostate gland; it is important to regularly undergo preventive examinations with a urologist-andrologist. So the risk will be minimal (read more about the prevention of prostatitis here).
Prostatitis is a complex and poorly understood disease. There are many more questions about him than answers. Understanding the many nuances on your own is, of course, difficult, even rather impossible. Specialist consultation required. Don't risk your sexual health. This is the most correct way.