Home >
Erectile Dysfunction >
MRI or trusion of the prostate
MRI or trusion of the prostate
Which is better than MRI or MRI of the prostate
Have you been struggling unsuccessfully with PROSTATITIS and POTENTITY for many years?
Head of the Institute: "You'll be amazed at how easy prostatitis can be cured by taking it every day.
If you have not heard about transrectal ultrasound of the prostate, that is, through the rectum (TRUS), then our publication was created especially for you. What is the purpose of such a procedure? How is TRUS made? Pros and cons of research. You will find answers to these and many other questions in our publication today.
Indications and contraindications for TRUS
Our readers have successfully used M-16 to improve potency. Seeing the popularity of this tool, we decided to bring it to your attention. Read more here-
Transrectal ultrasound of the prostate gland is prescribed at the first signs of prostatitis, potency disorders, infertility, pain in the perineum, as well as in case of painful defecation or constipation. If seals are found in the anus or in the prostate gland, TRUS is also prescribed.
Unlike conventional ultrasound, Transrectal ultrasound is considered more informative. The doctor has the opportunity to carefully examine the condition of many internal organs, as well as simultaneously perform a biopsy, that is, take cell samples for examination.
As for contraindications, this procedure, as a rule, is not performed with hemorrhoids in the acute stage, as well as after surgery on the rectum and with intestinal obstruction. However, if the patient's condition is critical, then TRUS is performed even if there are contraindications.
How is a transrectal examination performed?
This procedure requires preliminary preparation of the patient, therefore, a few days before it is carried out, it is necessary to exclude from the diet all products that cause increased gas formation. Legumes, peas, cabbage, yeast baked goods, pasta, fresh fruit, as well as carbonated drinks and alcohol are prohibited. For three days it is recommended to eat chicken meat or fish, boiled vegetables and soups, liquid cereals. On the eve of the study, the last dinner should take place before 19:00, and an hour and a half after a meal, you must take activated charcoal at the rate of 1 tablet per 10 kg of weight. Do a cleansing enema before going to bed. There is no breakfast on the day of the procedure.
If your doctor has ordered a transrectal ultrasound of the prostate for problems such as infertility, elevated PSA levels, or reduced potency, drink 3-4 glasses of water an hour before the examination and try not to urinate. If TRUS is to help find the cause of a urinary problem, it is best to come to the office with a bottle of water or tea 40 minutes before the scheduled time. As a rule, the patient begins to drink liquid right in the waiting room, and when he feels the urge to urinate, he tells the ultrasound doctor about it - and he invites him to the study room.
Please note that if the upcoming procedure causes you anxious and depressed emotions, then it is recommended to take mild sedatives - Valerian, Persen, Novopassit.
Usually TRUS lasts no more than 20 minutes. You will be asked to lie on your left side with your knees drawn up to your chest. There should be no pain during the procedure.
After examining the base of the prostate gland, the doctor proceeds to examine the seminal vesicles. If it is necessary to perform a biopsy, then before the TRUS procedure, the specialist gives the patient an anesthetic injection.
Advantages and disadvantages of the TRUS method
The advantages of transrectal ultrasound include the following:
- the procedure is non-traumatic and safe for men's health;
- this is a fairly informative diagnostic method that does not require additional research measures - analyzes or biopsy;
- TRUS replaces the x-ray, as it allows you to see all the soft tissues of the abdominal organs;
- this is a very quick way to diagnose.
As for the shortcomings of TRUS, the patient's mood plays a huge role here. Of course, for a man, any intervention in the genitals is a huge stress. However, do not forget that this is just a study necessary for health. The diagnostic doctor sees more than 10 patients a day, so you should not be shy and worry, but you just need to set yourself up for the fact that everything will be over in 20 minutes.
Good luck and great results!
The site map is an extremely convenient and effective tool for both quick navigation between sections of our web resource and for precise content search. The structure of the site is displayed in a tree form, which contributes to greater clarity and accessibility of various materials, even for novice Internet users.
Our readers have successfully used M-16 to improve potency. Seeing the popularity of this tool, we decided to bring it to your attention. Read more here-
Preparing for MRI of the prostate - the effectiveness of the procedure and its cost
Prostate MRI is an instrumental non-invasive diagnostic method. A magnetic resonance tomograph registers the slightest fluctuations of electromagnetic fields reflected from the organs and tissues of the human body. The result of studies of the prostate gland - pictures showing the layered state of its tissues. The final diagnosis is made by a specialist who analyzes the obtained images.
What the research shows
Magnetic resonance imaging of the prostate gland is indicated for suspicion of any of the pathologies of the organ. During the examination, the device may show the following deviations:
- inflammatory processes;
- the presence of a tumor - MRI accurately enough to determine its type;
- hypertrophic tissue changes;
- state of nearby vessels, lymph nodes, nerve endings;
- patency of the urinary and seminal tracts;
- possible damage to nearby tissues and organs of the small pelvis.
As a result of the examination, several pictures are obtained that show the condition of the prostate from different angles. Indications for MRI:
- diagnosis of chronic prostatitis;
- detection of prostatic hyperplasia;
- assessment of the anatomy of the organ to exclude congenital developmental anomalies;
- preparation for surgery;
- the presence of postoperative complications;
- an increase in the level of PSA - a tumor marker;
- prostate abscess on the background of prostatitis;
- suspicion of the occurrence of neoplasms - cysts and tumors.
MRI is considered one of the most informative instrumental research methods due to the possibility of diagnosing both the organ itself and nearby tissues. His pictures will show the slightest changes in the histological structure of the analyzed object. Diagnostics makes it possible to identify prostate diseases in the early stages.
Which is better: ultrasound, MRI, TRUS or biopsy
The advantages of magnetic tomography:
- safety - diagnostics do not require penetration into the body, and ionizing radiation does not harm even with frequent examinations;
- accuracy - detailed and clear MRI images allow you to see the slightest pathological changes in the prostate;
- low probability of error - other organs and systems rarely distort the image of the prostate gland, which is likely during ultrasound;
- informative - the ability to use various diagnostic methods allows you to most accurately assess the condition of tissues.
Comparison of magnetic resonance imaging with other methods:
- biopsy - allows with absolute probability to assess the structure of the neoplasm, the lack of the possibility of a full study of the prostate gland itself;
- Ultrasound is an informative method, performed through the anterior abdominal wall, less clear image detail than with MRI, low chance of accurately determining the type of tumor;
- TrUS - transrectal scanning is considered more accurate than a simple ultrasound, but requires penetration of the probe into the rectum; inability to identify the nature of the tumor.
MRI is performed before a biopsy, which significantly increases the efficiency of diagnosis. Fusion biopsy of the prostate involves targeted sampling of biomaterial under MRI control. This minimizes the risk of incorrect results and the need to repeat the biopsy.
Due to the information content of the method, MRI of the prostate is often prescribed for low information content of computed tomography, ultrasound and TruS.
How to prepare for research
Preparation for the study is necessary to obtain accurate results. The day before the MRI, the patient should:
- avoid eating foods that stimulate gas formation in the intestines;
- take medicine for bloating;
- cleanse the intestines with an enema or laxative;
- give up food for 4 hours;
- drink 0.5-1 l of water without subsequent emptying of the bladder - in 2 hours;
- take an antispasmodic - 30 minutes before.
In preparation for an MRI of the prostate, you should collect all available medical documentation. It can be useful in determining contraindications for diagnosis. You should bring a doctor's referral, a medical record, and the results of other recent imaging studies with you to the examination. Loose, comfortable clothing without metal buttons or zippers should be taken to the hospital. In its absence, some clinics issue their own gown.
If there are metal implants in the body, the patient must notify the attending physician and the specialist performing the procedure. If they are in the abdominal cavity or in close proximity to the small pelvis, MRI may be contraindicated.
Before the procedure, the patient prepares as follows: changes clothes, removes all metal objects from the body, including jewelry, removes dentures and a hearing aid. To relieve nervous tension, it is allowed to take a light sedative. All personal belongings remain outside the room where the diagnostics are carried out.
How long after a biopsy can I do an MRI of the prostate
After sampling the biomaterial of the prostate or its neoplasms, small hemorrhages form in the surrounding tissues and the gland itself. The results of instrumental methods of examination may be inaccurate. After prostate biopsy and other invasive procedures, MRI can be done after 20-30 days. This period is sufficient for the disappearance of local hemorrhages and complete healing of tissues. If the biopsy was performed in another medical institution, it must be reported to the doctor who prescribes magnetic resonance imaging.
How to do an MRI of the prostate
After the preparatory measures, the patient lies down on the working surface of the magnetic resonance tomograph. The table is immersed in a special cylinder until the area under study is in the center of the electromagnetic field. The patient may ask for headphones or ear plugs: the work of the tomograph is accompanied by a rhythmic hum. The equipment has a device for continuous communication between specialists and the patient.
While the diagnosis is being carried out, the man should lie still. To ensure the clarity of the images, the patient's body can be secured with special straps or cords. The procedure lasts 30-40 minutes. At the end of it, specialists are engaged in deciphering the images, and the patient can change clothes.
If it is necessary to study additional parameters of the prostate, separate types of magnetic tomography are used. The choice of method depends on the goals of the study, as well as the type of information that the doctor needs to make an accurate diagnosis and select treatment tactics.
Traditional method
In a classic MRI, the patient is simply immersed in the tomography camera, the pelvic region is scanned for half an hour. Fixing is not required. There are no additional requirements for the patient.
If more accurate diagnosis of the prostate gland is needed, MRI is done using a transrectal sensor. This device is a flexible wire immersed in a latex cuff. The coil is inserted into the rectum, so high-quality bowel cleansing on the eve of the procedure is a prerequisite. The cuff is inflated to secure the coil and prevent it from shifting during the procedure. The device creates an additional magnetic field directly near the gland, which provides increased clarity of images of tissues located deep in the body of a man.
With contrast
MRI of the prostate with contrast is done to improve the clarity of visualization of pathological tissues in the gland. It is used to assess the state of the vessels of the prostate, the rate of entry and removal of the coloring solution from the organ.
The technique requires additional preparation. The patient is checked in advance for allergic reactions to the injected solution, the state of the kidneys is examined (in any form of insufficiency, the use of contrasts is prohibited). Just before the scan, a contrast agent is injected into a man's vein. It instantly spreads throughout the body and settles in pathological cells. This makes them more visible to the MRI scanner.
In a dynamic study with contrast, the solution is administered drip after preliminary mixing with isotonic sodium chloride solution. Thus, the substance enters the patient's body directly during the operation of the tomograph.
Multiparametric MRI
This type of diagnostics combines all possible methods of conducting magnetic resonance scanning. The procedure requires thorough preparation, including ultrasound of the kidneys, tests for allergic reactions, bowel cleansing. It differs from other methods of this examination by a longer duration. Includes several parameters - dynamic contrast, spectroscopic and diffuse-weighted studies.
Multiparametric MRI of the prostate is characterized by high accuracy and minimal risk of error. During the procedure, specialists receive a multidimensional image of the gland. Comprehensive MRI detects even single atypical cells, diagnosing tumors at the stage of their inception. Allows you to avoid a biopsy due to a reliable determination of the type of neoplasm.
MRI for prostate tumor
MRI is the main and most accurate way to diagnose prostate cancer in men.The image shows formations of any size and density, it is possible to evaluate their chemical composition. Targeted MRI of the prostate allows you to identify inflammatory changes and tumors of minimal size, for this, the examination is carried out on high-precision tomographs. The course of oncology with the help of this diagnosis is detected already at the 1-2nd stages.
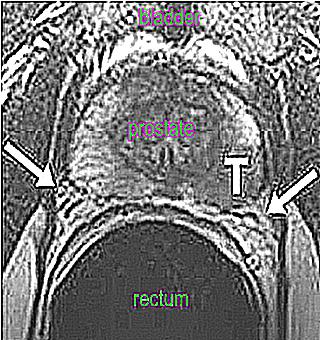
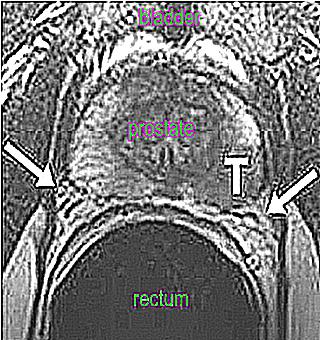
The image clearly shows the structure, size and shape of the formations, the clarity of the boundaries. A rupture of the walls of the tumors and the exit of atypical cells outside the prostate are revealed. The pictures show the smallest metastases of the tumor in soft tissues and bone structures. With the help of a contrast study, it is possible to determine the degree of malignancy of the gland, the activity of its blood supply. To evaluate the results, doctors use the PIRADS scale.
Results
Prostate MRI results - multiple images of the organ in different projections. Focusing on them, the doctor evaluates the location, size and shape of the prostate, seminal vesicles, bladder, lymph nodes and other nearby tissues.
An overall picture of the condition of the gland can be obtained from MRI scans of the testicles, bladder, or other organs of the small pelvis.
Pathologies are identified by the intensity of visible shadows, their shape, and the clarity of the boundaries. With prostatitis, cone-shaped foci of low staining intensity indicate the course of the inflammatory process. Areas of hyperplasia are found in prostate adenoma. Asymmetrical bulging of the borders of the prostate gland, asymmetry of the neurovascular bundles, and foreign inclusions in adjacent tissues speak of a malignant neoplasm. The results of the study should be evaluated by a urologist, surgeon or oncologist. The radiologist performing the procedure can only make a preliminary diagnosis.
Research cost
The cost of the procedure depends on the type of technique, the model of the tomograph, and the qualifications of the radiologist.
MRI of the prostate. Who did? How informative is TRUS?
MRI of the prostate. Who did? How informative is TRUS?
1 Post by duba " Fri Jan 12, 2018 11:21 am
MRI of the prostate. Who did? How informative is TRUS?
2 Posted by Anton UG " Fri Jan 12, 2018 1:41 pm
MRI of the prostate. Who did? How informative is TRUS?
3 Post by GrisGrey " Fri Jan 12, 2018 6:32 pm
MRI of the prostate. Who did? How informative is TRUS?
4 Post by avrok " Fri Jan 12, 2018 7:51 pm
MRI of the prostate. Who did? How informative is TRUS?
5 Posted by GrisGrey " Fri Jan 12, 2018 8:40 pm
MRI of the prostate. Who did? How informative is TRUS?
6 Post One man " Sat Jan 13, 2018 4:10 pm
MRI of the prostate. Who did? How informative is TRUS?
7 Posted by Anton UG " Sun Jan 14, 2018 12:47 am
MRI of the prostate. Who did? How informative is TRUS?
8 Posted by neponyatno " Sun Apr 01, 2018 10:04 pm
Who did it with contrast? It seems like I want to, but I've read horror stories. I'm striving. My creatinine is 106 according to the latest analysis, my kidneys are not a fountain.
And the second question: who did an MRI (any) did they find anything at all?
MRI of the prostate. Who did? How informative is TRUS?
9 Posted by vaxell " Sun Apr 01, 2018 11:28 pm
Neponyatno wrote: Who did with contrast? It seems like I want to, but I've read horror stories. I'm striving. My creatinine is 106 according to the latest analysis, my kidneys are not a fountain.
And the second question: who did an MRI (any) did they find anything at all?
MRI of the prostate. Who did? How informative is TRUS?
10 Post by neponyatno " Sun Apr 01, 2018 11:36 pm
MRI of the prostate. Who did? How informative is TRUS?
11 Posted by neponyatno " Tue Apr 03, 2018 4:48 pm
In short, I did a 3T MRI today, I'll take the conclusion over the weekend, but it seems like they always didn't find anything.
From the unusual: during the procedure itself, when the small pelvis was scanned, there were precisely those pain sensations on the left side that usually bother me. Strong enough.
In general, most likely the vas deferens or some tissue around the seminal vesicle is inflamed. Do not know. I'll try 1 more course of ATB, it can't be worse
Learn how to cure prostatitis
Recovery starts today.
Detailed and accessible information about modern methods of diagnosing and treating diseases of the prostate
- Identification of causes
- Suppression of infections in the prostate
- Methods of treatment
- How not to get sick again and others