Home >
Erectile Dysfunction >
Treatment methods for chronic prostatitis
Treatment methods for chronic prostatitis
In addition to acute bacterial prostatitis, there are other forms:
- chronic prostatitis of bacterial origin;
- non-bacterial chronic prostatitis;
- asymptomatic prostatitis.
Chronic bacterial prostatitis
Chronic prostatitis of bacterial origin is an inflammation of the prostate gland with a gradual onset, caused by an infection, usually of a persistent nature.
Compared to the acute form, chronic bacterial prostatitis is a milder disease, but has a much longer duration (at least 3 months).
Reasons
Chronic bacterial prostatitis can be:
- due to untreated bacterial acute prostatitis;
- the result of urinary tract infections (urethritis, cystitis, etc.);
- complication of testicular infection (epididymitis).
Risk Factors
Increase the risk of developing chronic bacterial prostatitis:
- using a bladder catheter (bladder catheterization);
- presence of an infection in the urinary tract;
- presence of urethral stenosis;
- infection in the testicles;
- benign prostatic hypertrophy (or enlarged prostate);
- negligence in the treatment of acute bacterial prostatitis;
- urinary tract injury;
- systemic infections.
Complications
In the absence of proper treatment, a number of complications can arise:
- inability to urinate;
- the formation of an abscess of the prostate gland. This is a very rare complication;
- bacteremia or, in particularly unfortunate cases, sepsis.
Diagnostics
As a rule, the diagnostic route to identify chronic bacterial prostatitis and its exact causes begins with an objective examination, followed by a thorough history; therefore, it continues with the so-called digital rectal analysis (ERD) and palpation of the inguinal lymph nodes; finally, it ends with a blood test, urinalysis, laboratory analysis of prostate fluid obtained after massage of the prostate gland, urethral smears aimed at detecting sexually transmitted infections, urodynamic examination, cystoscopy and ultrasound of the urinary tract.
Digital Rectal Analysis (ERD)
During this analysis, the thought of which terrorizes many patients, a doctor (usually a urologist) manually analyzes the health of the prostate gland by gently inserting fingers into the rectum, well lubricated and protected by a glove. Since the prostate is located directly in front of the rectum, the examiner can touch the upper surface of the prostate gland. If this surface is enlarged, tender and painful, it is very likely that the prostate is inflamed or, in any case, not in full health.
Therapy
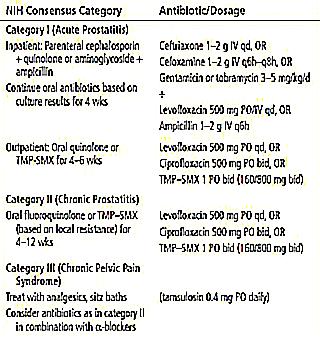
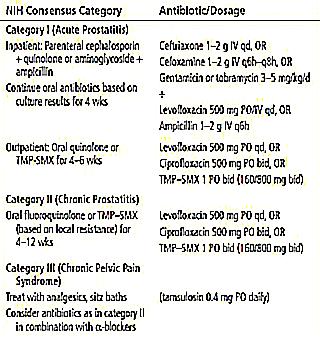
Similar to the treatment of the acute form, the treatment of chronic bacterial prostatitis consists of special antibiotic therapy.
It can be said that effective treatment of Chronic prostatitis is difficult for at least two reasons:
- Low sensitivity of the prostate gland to antibiotics. As readers will recall, this characteristic of the prostate is also an obstacle to the treatment of acute bacterial prostatitis. Among the antibiotics that are best able to spread and concentrate in the prostate gland are the quinolones (ofloxacin, ciprofloxacin, and norfloxacin); all other antibiotics are not suitable;
- Relapse, which characterizes chronic inflammation of the prostate gland, especially of bacterial origin.
To minimize the risk of relapse, it is important to follow your doctor's recommendations for the duration of antibiotic therapy and the best ways to take your medication.
What is the specific duration of antibiotic therapy?
The duration of antibiotic therapy varies from patient to patient, in some cases, 6-8 weeks of therapy is sufficient; otherwise it will take 12 weeks (3 months) or 6 months.
Typically, when antibiotic therapy lasts 5 to 6 months, medications are applied for 2-3 weeks for each month of treatment.
How to relieve symptoms
To relieve some of the symptoms of chronic bacterial prostatitis, especially pain, doctors advise:
- take hot baths;
- drink plenty of water (2 liters per day);
- avoid drinking alcohol;
- reduce or, better yet, avoid coffee, orange and citrus juices, hot and especially spicy foods;
- take pain relievers and anti-inflammatory drugs such as paracetamol or ibuprofen;
- avoid using a bicycle;
- use decongestant herbal remedies (decoctions and infusions infused with gram, parsley cornel, artichoke leaves, sage, birch, ursine or dandelion).
Treatment of complications
Formation of a prostate abscess requires a minor surgical procedure to drain the pus.
Bactemia and sepsis require additional antibiotic therapy, which must be administered in a hospital under close medical supervision. Bacteria and sepsis are two medical emergencies and as such require the immediate intervention of experienced professionals in the field.
Finally, the inability to urinate forces patients to use a catheter to empty their bladder.
Prevention
For the prevention of chronic bacterial prostatitis it is important:
- drink water in quantities that meet the needs of the body;
- take care of intimate hygiene;
- so that the remedy quickly treats urinary tract infections.
Chronic non-bacterial prostatitis
Known and classified in the 1960s as prostatodynia, chronic nonbacterial prostatitis is the most common form of inflammation in the male population.
The exact reasons are unclear at this time; however, they still highlight:
- problem of nerve endings (nerves) of the prostate gland;
- autoimmune character; in other words, it depends on a malfunction of the immune system, which recognizes the prostate as foreign and attacks it;
- special circumstances such as trauma to the prostate gland, excess stress, daily heavy lifting and intense exercise.
As a rule, to diagnose chronic non-bacterial prostatitis, doctors do the same exams and laboratory tests as in the case of suspected bacterial prostatitis. Moreover, the only way to know which form of inflammation is in question is to look for bacteria in the blood, urine, and prostatic fluid. The absence of bacteria in these organic fluids, combined with the typical symptoms of prostate inflammation, is militant in favor of non-bacterial chronic prostatitis.
Currently, there are no specific treatments for this form of the disease, but only symptomatic means. Once again, we can add that the effective treatment of chronic prostatitis is quite complicated.
Among these symptomatic remedies for prostatitis, effective:
- administration of alpha-blocking drugs. Alpha blockers are supposed to relieve symptoms by releasing smooth muscle in the prostate and bladder;
- administering pain relievers such as paracetamol or NSAIDs;
- introduction of laxatives. Several clinical studies have shown that the use of laxatives in several patients with chronic non-bacterial prostatitis led to an improvement in symptomatic structure.
In fact, it needs to be clarified that for many years there has been a discussion about the use of antibiotics to treat some chronic forms of the disease: for some doctors antibiotic therapy is good, for others it is useless, even potentially dangerous.
Many chronic conditions that cause persistent pain are difficult to treat in certain ways and tend to recur occasionally, chronic nonbacterial prostatitis is often responsible for episodes of depression and anxiety.
Potential solutions for coping with depression and anxiety from chronic persistent pain, according to doctors, include support groups for people with similar disorders and the use of natural antidepressants.
Formulating a prognosis for chronic non-bacterial prostatectomy is very difficult, since this condition manifests itself differently from patient to patient:
- in some men, the symptomatic structure improves significantly within about 6 months of therapy;
- in other men, symptomatic improvement is moderate and does not go away until a year of treatment; in others, symptoms and signs disappear indefinitely.
Traditional medicine
Natural traditional medicines appear to relieve symptoms of chronic nonbacterial prostatitis:
- using a pillow in a long sitting position;
- hot baths;
- avoid spicy foods, coffee and alcoholic beverages;
- acupuncture;
- relaxation exercises;
- drink blueberry juice;
- massage;
- herbal medicine.
Asymptomatic prostatitis is an inflammation of the prostate gland that does not cause any symptoms in men. Doctors have not yet understood the reason why this condition is asymptomatic. As a rule, asymptomatic prostatitis does not require any treatment.