Home >
Erectile Dysfunction >
How to treat an acute form of prostatitis
How to treat an acute form of prostatitis
Acute prostatitis in men: symptoms and treatment
Acute and chronic prostatitis are the most common male diseases. In clinical urology, these diseases are diagnosed in 30-60% of men of reproductive and working age (30-50 years).
Acute prostatitis is an inflammatory lesion of the prostate gland, accompanied by edema and the formation of purulent foci in the tissues of the prostate. The disease is caused by exposure to various pathogenic microorganisms.
The disease does not require emergency treatment. However, ignoring acute inflammation can lead to the fact that it becomes chronic. Therefore, when the first symptoms occur, you should consult a doctor and get an appointment for treatment.
Causes of disease
Most often, the disease affects men over the age of 30 years. The causes of its occurrence are usually associated with the negative impact of various pathogenic microflora. Among the microorganisms that can lead to the appearance of symptoms of acute prostatitis, there are:
- Escherichia coli and Pseudomonas aeruginosa;
- Staphylococcus aureus;
- enterococcus;
- Klebsiella;
- Proteus
Many of the bacteria are in the body all the time. But in the normal state, they do not lead to the appearance of an inflammatory process. When they penetrate the mucous membrane of the prostate gland through the urethra, they begin to actively multiply and cause a strong inflammatory process.
Some bacteria enter the body through unprotected intercourse. Therefore, men who do not use contraceptives and constantly change partners suffer from the disease especially often.
There are also non-infectious causes of the inflammatory process. Among them are:
- inactive (sedentary) lifestyle;
- overweight;
- unhealthy composition and diet;
- severe hypothermia;
- insufficient sexual activity;
- coitus interruptus;
- smoking;
- excessive drinking.
All these factors (individually or in combination) lead to stagnation of secretion in the prostate gland and blood in the vessels located next to the organ.
The accumulation of secretion creates favorable conditions for the reproduction of pathogenic microorganisms, which causes an inflammatory process. And in turn, the latter can cause a variety of complications from abscess and prostate adenoma to prostate cancer. Often men have problems with potency and conceiving children.
Symptoms and forms of the disease
When Acute prostatitis occurs in men, the symptoms may vary. The severity of the manifestations of the disease depends on the stage and form of the inflammatory process in the prostate gland.
At the initial stage of the onset of the disease, a subacute form of the disease may be noted. Its symptoms are very weak. This is due to the low activity of pathogens or a good level of body resistance. The disease is very difficult to diagnose. Therefore, treatment may not be timely. And then the disease goes through several stages: catarrhal, follicular, parenchymal.
The clinical manifestations and symptoms of acute prostatitis correspond to the stages of the process. Common manifestations are pain, urination disorders and intoxication.
Catarrhal form
When the infection enters the excretory ducts, a catarrhal form of acute prostatitis is observed. In this case, the pathogenic microflora affects the mucous membrane without penetrating into the deep layers of the organ. Inflammatory foci appear in the prostate, it swells and increases in size. There is also squeezing of the urethra. Often, such signs appear under the influence of the influenza virus.
Mild symptoms still appear as:
- minor urinary problems;
- more frequent urination, especially at night;
- heaviness in the perineum in a sitting position;
- increase in body temperature to 37-38C.
At the same time, hyperthermia and subfebrile condition are sometimes completely absent.
Symptoms of acute inflammation of the catarrhal form may disappear on their own after 14 days. However, treatment is not always required. However, in this case, there is a high probability that the disease will become chronic.
Treatment started in the catarrhal stage of acute prostatitis leads to recovery in 7-10 days.
Follicular form
In the absence of treatment of the catarrhal type of the disease, the appearance of a follicular form is observed. During this period, there is a spread of infection, damage to individual lobes of the prostate.Symptoms become pronounced and manifest as:
- acute pain when urinating;
- dull aching pain in the perineum radiating to the penis, anus or sacrum;
- difficulty in debugging due to severe pain;
- increase in body temperature up to 38C;
- complications of urination.
At this stage, a purulent lesion of the prostate is observed, as evidenced by the threads of pus in the urine.
With vigorous therapy of follicular prostatitis, after 12 days, complete elimination of the signs of the disease can be noted. Otherwise, it goes into the next more difficult stage.
Parenchymal form
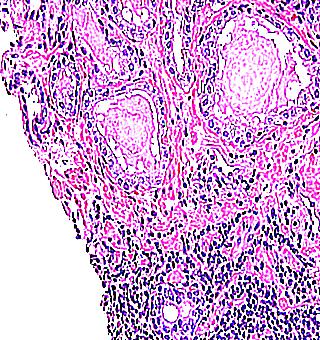
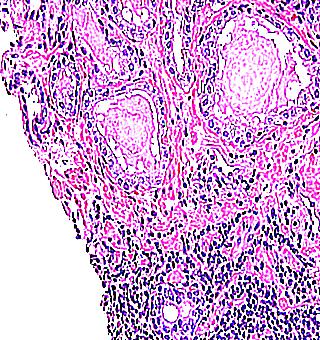
The diffuse or parenchymal form is the final stage of acute prostatitis. The inflammatory process extends to the parenchyma of the organ, where purulent foci are formed. Sometimes there is a complete lesion. The gland increases significantly in size.
The symptoms of this form are very pronounced:
If the treatment of acute prostatitis in the parenchymal stage is started on time, then the prognosis for a complete cure is favorable. Otherwise, the disease will become chronic or a prostate abscess will form.
Disease diagnosis
Diagnosis and staging of acute inflammation of the prostate is carried out by a urologist and is based on a comprehensive physical, laboratory and instrumental examination of the patient.
Examination of the prostate through the rectum allows you to determine the size, consistency, homogeneity, symmetry of the gland, pain reaction, foci of destruction, signs of purulent fusion of tissues.
In the obtained secret of the prostate, an increase in the number of leukocytes and amyloid bodies, a decrease in the number of lecithin grains are found.
There is also increased leukocyturia in the third portion of urine.
To isolate the causative agent of acute prostatitis and find out its cause, it is necessary to carry out:
- urine culture and urethral discharge with antibiogram;
- PCR studies of scrapings;
- blood culture for blood culture.
The nature and severity of dysuric disorders in the acute course of the disease is assessed using uroflowmetry.
Ultrasound of the prostate gland with moderate pain syndrome can be performed transrectally, and in case of severe pain reaction - transabdominally. The shape, size of the gland, the presence of focal or diffuse changes are evaluated echoscopically, the stage of an acute inflammatory process is established.
When planning a surgical operation for destructive forms of acute prostatitis, it is advisable to conduct an MRI of the pelvic area.
Treatment of disease
The leading role in the treatment of acute prostatitis belongs to etiotropic therapy. It is necessary to prescribe antimicrobial (antibacterial, antiviral, antitrichomonas, antimycotic) drugs as early as possible to suppress the reproduction of microorganisms in the gland and tissues of the urethra.
In order to reduce spasms and painful urination, analgesics, antispasmodics, rectal suppositories with anesthesin or belladonna, thermal microclysters are prescribed. In the complex therapy of acute prostatitis, NSAIDs, enzymes, immunomodulators, vitamins, infusions of solutions are used.
Physiotherapy for acute prostatitis is carried out after the acute symptoms subside.
Diet plays an important role in therapy. Also, during the treatment period, it is worth drinking plenty of fluids. This helps to ease the process of urination and relieve pain.
Folk recipes can also help speed up the healing process.
Medicines
The treatment of acute prostatitis is aimed at eliminating the infection that caused inflammation, as well as normalizing blood circulation and eliminating congestion. It is usually done on an outpatient basis. Hospitalization may be required for patients with parenchymal disease.
In acute infectious prostatitis, therapy necessarily includes taking antibiotics. The duration of therapy and the drugs used in this case should be prescribed exclusively by a specialist.
Different antibiotics are effective against different microorganisms. Therefore, the doctor must evaluate the result of sowing and choose a remedy that will help to cope with the infection that provoked the disease. Usually treatment is carried out with:
Fluoroquinolones are recognized as the most effective in inflammation of the prostate. Therefore, they are often prescribed in the acute course of the disease.
In addition to antibacterial drugs, antihistamines (Zirtek, Zodak, Suprastin) and intestinal bacteria (Lactobacterin, Bifidumbacterin, Linex) are prescribed.
During the treatment period, it is necessary to maintain immune protection at the proper level.For this purpose, the following drugs are prescribed:
Timalin (promotes the restoration of gland tissues); Taktivin (indispensable in the presence of purulent foci); SIAM (good for bacterial damage).
You may also need to take interferons. They are used in the form of rectal suppositories and intramuscular injections. Among them, high efficiency is noted:
Physiotherapy
After the signs of the acute stage of the disease subside, you can undergo physiotherapy. It is necessary to eliminate the inflammatory process, relieve swelling of the gland tissues, eliminate pain, improve microcirculation and increase local immunity.
Common methods of influence are:
- rectal electrophoresis;
- UHF therapy;
- UHF therapy.
Prostate massage is also effective.
The diet for prostate inflammation is based on the principles of a healthy diet and limiting the intake of junk food. The diet is selected taking into account the severity of the manifestation of the disease and the characteristics of the organism.
During the treatment period, you should stop using:
- fatty meat and fish;
- salty and spicy food;
- preservation products;
- smoked meats;
- cabbage;
- legumes;
- strong tea and coffee;
- alcohol.
It is worth enriching the diet with fermented milk products, cereals and juices.
An element such as zinc plays an important role in the treatment of inflammation of the prostate. It is contained in:
- chicken meat;
- eggs;
- pumpkin seeds;
- walnuts.
During the treatment period, it is imperative to consume a large amount of liquid. In this case, you must completely abandon the intake of alcoholic beverages. They slow down the healing process, provoking various complications.
Folk recipes
Doctors believe that it is impossible to cure the disease with the help of folk remedies. But to alleviate the patient's condition in the acute course of the disease with their help is completely realistic. After all, even many medications are made on the basis of medicinal plants, which are widely used in traditional medicine recipes.
A specialist can advise the use of decoctions and infusions of medicinal herbs and plants. They are taken orally or added to water during sitz baths. Among the useful plants are:
- aspen bark;
- chestnuts;
- horsetail;
- chamomile;
- coltsfoot;
- oak bark.
It is worth remembering that some herbs can cause allergic reactions. Therefore, you should not prescribe them on your own. Otherwise, you can provoke the appearance of various complications.
The acute form of prostatitis is quite amenable to therapy. It is important to start it in a timely manner when the first symptoms occur. If delayed with therapy, the disease can become chronic. In this case, it will be much more difficult to cure it.
Useful video
Symptoms and treatment of acute prostatitis in men how to relieve an attack with antibiotics and folk remedies
Every second man of reproductive age (up to fifty years old) is prone to such a delicate disease as acute prostatitis, in which, under the influence of certain factors, the prostate (prostate gland) becomes inflamed, causing various forms of disorders of sexual functions, fertility, and psycho-emotional states. Be attentive to what your body says, and do not neglect timely treatment.
What is acute prostatitis
If a man feels discomfort and even pain during urination, you should immediately consult a doctor, because acute prostatitis is a disease of infectious etiology that causes inflammation of the prostate, followed by the formation of edema of the glandular tissue, the formation of purulent foci on it. If you do not pay attention to the signs of acute inflammation of the prostate, then the pathological process can transform into a chronic form that is difficult to treat, and there is very little time for reflection, the transformation occurs in a matter of days.
However, more serious complications are possible than its transition to a chronic form. There is a risk of sepsis - a general infection of the blood and an ascending infection of the urinary tract with the development of pyelonephritis and cystitis. In these cases, the patient is urgently hospitalized, the condition may be critical. Although sepsis as a complication is rare, it can occur in patients in immunosuppressive conditions - intoxication, fever, severe symptoms, weakness. Therefore, blood cultures are needed to detect microorganisms.
Symptoms of acute prostatitis
Every man needs to know and remember the symptoms of acute prostatitis. General signs of the disease appear:
- Sharp pain when urinating.
- Intoxication of the body.
- Impaired urination (intermittent, weak, strained stream).
- Frequent urge to go to the toilet at night.
These are external symptoms of prostatitis, but with a deeper examination, leukocytes, traces of mucus and pus in the secretory fluid of the prostate gland are found in the urine. On palpation, a dense, enlarged organ is felt, pressing will be painful. Further development of the inflammatory process is characterized by heaviness and pain in the perineum, radiating to the penis, sacrum and rectum. As a result, it becomes difficult for the patient to empty the bladder and defecate due to severe pain. Body temperature can rise up to 38C.
Causes of acute prostatitis
Since this disease is bacterial inflammatory in nature, the following infectious agents are the causes of acute pancreatitis:
Microbial microflora penetrates into the glandular tissue of the prostate, as a rule, by the transcanalicular route (through the urethra and excretory ducts of the prostate gland). In cystitis, the infection migrates to the prostate from the bladder. Other possible routes of bacteria penetration are opened during endourethral manipulations (catheter placement, urethral bougienage, cystoscopy, ureteroscopy). Pathogenic microorganisms migrate into the prostate from distant pathogenic foci in caries, sinusitis, tonsillitis, cholecystitis, pyoderma, bronchitis.
There is a high probability of infection from the intestines with proctitis, hemorrhoidal fissures, colitis. Non-infectious factors that can cause an attack of prostatitis are congestive (congestive) venous phenomena in the pelvic area and impaired drainage of the acini of the gland. Congestion can be caused by irregular or, conversely, excessive sexual activity, interruption of sexual intercourse, a sedentary lifestyle, frequent constipation, frequent alcohol intoxication, varicose veins of the small pelvis, hypothermia.
Forms of acute prostatitis
The clinical development of this disease is considered in three stages, which at the same time are forms of acute pancreatitis. This is:
Acute prostatitis in men begins with catarrhal inflammation, which is characterized by the expansion of the acini, the occurrence of edema of the glandular tissue and, as a result, an increase in the size of the organ. The excretory ducts of the prostate glands, which open into the posterior urethra, are actively involved in the inflammatory process. The lobules and ducts of the prostate gland become inflamed, their contractility is disturbed, they narrow and clog, this can make it difficult to secrete the prostate secretion.
At the catarrhal stage, the pathological process stops at the mucous layers and does not go deeper. In the process of progression, the disease spreads to the entire prostate gland. Follicular acute bacterial prostatitis develops. At the analysis in urine pus comes to light. The tissues of the gland destructively change, swelling continues to increase. The follicular form is still relatively easy to treat.
Further, a parenchymal form of the disease develops, the outcome of which can be an abscess of the prostate, that is, chronic prostatitis. Therefore, symptoms such as:
- Increase in body temperature up to 39C and above.
- Manifestations of intoxication: weakness, chills, thirst, lack of appetite.
- Frequent urges to the toilet for small needs are accompanied by throbbing sharp pains.
- Inability to empty the bladder.
- Meteorism.
- Tenesmus.
- Constipation
- Discharge of mucus from the anus.
Diagnosis of acute prostatitis
At the first suspicion of inflammation of the prostate gland, hurry to the doctor. Correct and comprehensive diagnosis of acute prostatitis is very important for quick and successful treatment. The doctor will first analyze the history, clarify when pain sensations appear in the perineum, whether they increase or decrease during ejaculation, urination, defecation. Be sure the doctor must study the patient's medical history: what diseases were transferred, whether there were sexually transmitted infections.
The urologist will palpate the external genital organs to determine developmental pathologies, visible signs of prostatitis, and rectal examination - palpation of the prostate gland through the anus. To create a complete clinical picture, it will be necessary to undergo the following examinations:
Treatment of acute prostatitis
After a thorough diagnosis, they begin the treatment of acute prostatitis. It is based on antibiotic therapy, the purpose of which is to suppress infectious pathogens. Additionally, conservative treatment of prostatitis includes the use of:
- Anti-inflammatory drugs.
- Means that improve blood circulation.
- Painkillers and antispasmodics.
- Medicines that support metabolic processes in the prostate.
- Multivitamins
- Phytotherapeutic agents.
- Immunomodulators
The advanced forms of inflammation of the prostate with the appearance of purulent foci require surgical intervention. Transurethral (through the wall of the urethra) or transrectal (through the wall of the anus) drainage of abscessed areas is performed. Surgery may be required in case of pathological urinary retention
Drugs
Treatment of acute prostatitis in men with drugs (tablets, injections) is the basis of successful therapy. With well-prescribed antibiotic therapy, the infection can be overcome in a few days. However, it is recommended to continue treatment for four weeks in order to achieve complete eradication of the pathogenic microflora. Medications used in the disease are:
- Etiotropic (antibiotics) - destroying pathogens.
- Pathogenetic (NSAIDs) - eliminating congestion in the prostate.
- Symptomatic (analgesics, antipyretics) - relieving pain, muscle spasms of the organ, and other symptoms.
For the treatment of inflammation of the prostate, the doctor may prescribe a set of drugs, which will include:
- Injections - contribute to the penetration of the drug into the tissues of the organ in a short time.
- Suppositories (rectal) - analgesic, antibacterial effect.
- Microclysters with herbal decoctions.
- Broad-spectrum antibacterials, unless a specific causative agent is identified.
Antibiotics for acute prostatitis
The main causative agents of prostatitis are pathogenic bacteria that cause inflammation in the tissues of the prostate gland. Therefore, antibiotics for acute prostatitis are the basis of treatment and are prescribed only after testing for the sensitivity of the microflora. Antimicrobials used for inflammation are divided into the following groups:
Prevention of acute prostatitis
In order for a man to be always healthy, full of strength, the prevention of acute prostatitis is important, including:
It is important to completely cure diseases of the genitourinary organs (urethritis, cystitis, pyelonephritis, balanoposthitis). Undertreated diseases can cause the development of an inflammatory process in the prostate gland. Among other things, we must not forget about increasing physical activity. In the cold season, hypothermia should be avoided. Prostate massage is very useful for men's health. However, if the disease has already made itself felt, massage is contraindicated and even impossible due to the soreness of the organ.
Video: Signs of acute prostatitis
Acute prostatitis
Acute prostatitis is an infectious and inflammatory lesion of the prostate gland, accompanied by edema and the formation of purulent foci in the tissues of the prostate. Manifestations of acute prostatitis depend on the stage (catarrhal, follicular, parenchymal, abscessing) and may include dysuric disorders, pain in the perineum, fever, intoxication. Diagnosis is based on palpation of the prostate, ultrasound and dopplerometry of the prostate gland, examination of the discharge of the urethra and secretion of the prostate. Treatment of acute prostatitis includes the appointment of antimicrobial therapy, NSAIDs, antispasmodics, analgesics, immunomodulators, physiotherapy.
Acute prostatitis
Acute and chronic prostatitis are the most common and socially significant male diseases. In clinical urology, prostatitis is diagnosed in 30-58% of men of reproductive and working age (30-50 years). The course of acute prostatitis is accompanied by disorders of sexual function and fertility, disorders of the psycho-emotional state and social maladaptation.
Causes of acute prostatitis
The causative agents of acute prostatitis are predominantly non-specific infectious agents that penetrate into the tissues of the prostate - gram-negative (E. coli, Klebsiella, Proteus) or gram-positive (staphylococci, enterococci, streptococci). Often, acute prostatitis can be caused by pathogens of urogenital infections - chlamydia, trichomoniasis, ureaplasmosis, gonorrhea, mycoplasmosis, candidiasis, etc.
Most often, the penetration of microbial agents into the tissues of the prostate occurs in a transcanalicular way - through the excretory ducts of the gland, which open in the wall of the posterior urethra. Therefore, urethritis of any origin is very often complicated by acute prostatitis. Less commonly, microbial flora enters the prostate from the bladder in acute cystitis. The introduction of pathogens into the gland is greatly facilitated with increased intraurethral pressure (strictures, urethral stones), endourethral manipulations (urethral bougienage, bladder catheterization, ureteroscopy, cystoscopy, etc.).
In addition, acute prostatitis may be the result of hematogenous penetration of infection, which is facilitated by the conditions of blood supply to the prostate with a well-developed system of arterial and venous anastomoses. With hematogenous drift, microbes can enter the tissues of the prostate from distant purulent foci with tonsillitis, sinusitis, caries, cholecystitis, bronchitis, pyoderma, etc. Lymphogenous infection of the prostate gland from the intestine is possible with anal fissures, proctitis, colitis.
Non-infectious factors contributing to the development of acute prostatitis include persistent congestive (stagnant) phenomena in the pelvic veins and impaired drainage of the prostate acini. Congestion can be caused by dysrhythmia of sexual life and sexual disorders - the practice of coitus interruptus, the absence or irregularity of sexual activity, excessive sexual activity, etc. mainly alcohol) intoxication, varicose veins of the pelvis.
Forms of acute prostatitis
In the development of acute prostatitis, 3 forms are distinguished, which are at the same time its stages - catarrhal, follicular, parenchymal, abscessing.
Acute prostatitis begins with catarrhal inflammation - changes in the mucous and submucosal layer of the excretory ducts of individual lobules of the gland. In the future, swelling of the walls of the ducts contributes to the stagnation of the mucopurulent secretion in the prostate follicles and the progression of inflammation, in connection with which focal suppuration of the lobules can develop - acute follicular prostatitis. With multiple lesions of the lobules and diffuse involvement of the parenchymal and interstitial tissue of the prostate in the purulent-inflammatory process, acute prostatitis passes into its next stage - parenchymal. In the case of the fusion of small abscesses into a large focus, an abscess of the prostate gland is formed, which can open into the urethra, perineum, rectum or bladder.
Symptoms of acute prostatitis
Clinical manifestations in acute prostatitis correspond to the stages of the process. Common manifestations are pain, urination disorders and intoxication.
In the acute catarrhal stage of prostatitis, there is heaviness and pain in the perineum. Dysuric disorders are characterized by a painful increase in urination, especially at night. Body temperature remains within the normal range, may be slightly elevated; there is no intoxication. On palpation examination, the prostate is not changed or slightly enlarged, somewhat painful. Examination of the secret of the prostate reveals an increase in leukocytes, an accumulation of mucopurulent filaments. White blood cells appear in the urine when emptying the excretory ducts of the acini. prostate massage is usually not possible due to pain. Treatment started in the catarrhal stage of acute prostatitis leads to recovery in 7-10 days.
The follicular form of acute prostatitis is more pronounced, accompanied by dull aching pains in the perineum, radiating to the penis, anus or sacrum. Against this background, urination is painful and difficult, up to the development of acute urinary retention. The act of defecation in acute follicular prostatitis is also difficult due to severe pain. In view of the increase in body temperature to 38C, the general condition is disturbed. Palpation per rectum is determined by an enlarged, dense, tense, asymmetric prostate, sharply painful in some areas during digital examination. Urine collected after palpation of the gland contains a large amount of leukocytes and purulent filaments that form a cloudy sediment. Carrying out massage to obtain a secret of the prostate in the follicular stage of acute prostatitis is contraindicated. With vigorous treatment, acute follicular prostatitis may resolve favorably; otherwise, it proceeds to the next, parenchymal stage.
The clinic of acute parenchymal prostatitis is developing rapidly. Characterized by severe hyperthermia (up to 39-39.5 C and above) with chills, general weakness, appetite suppression, thirst. At first, urination is sharply accelerated and difficult, then it may stop altogether. Attempts to empty the bladder or intestines are accompanied by intense pain. Excruciating tenesmus, constipation, flatulence develop. The pain spreads to the rectum, is pulsating in nature, makes the patient take a forced position - lying with his legs tucked in. With the development of reactive inflammation of the rectum, mucus is released from the anus.
On palpation, a diffusely enlarged, with indistinct contours of the gland is determined, extremely painful at the slightest touch. Prostate massage in the parenchymal stage of acute prostatitis is contraindicated categorically. Sometimes, due to a sharp swelling of the pararectal tissue and pain, a rectal examination cannot be performed. In the urine - a pronounced leukocytria, pyuria.The outcome of acute parenchymal prostatitis can be the resolution of the disease, the formation of a prostate abscess or chronic prostatitis.
Diagnosis of acute prostatitis
Recognition and staging of acute prostatitis is carried out by a urologist (andrologist) and is based on a comprehensive physical, laboratory and instrumental examination. The study of the prostate through the rectum allows you to determine the size, consistency, homogeneity, symmetry of the gland; pain reaction, foci of destruction, signs of purulent fusion of tissues. In the resulting secret of the prostate, an increase in the number of leukocytes and amyloid bodies, a decrease in the number of lecithin grains are found.
In acute prostatitis, there is increased leukocyturia in the third portion of urine and in the urine collected after palpation of the prostate. To isolate the causative agent of acute prostatitis, it is necessary to carry out bakposev of urine and urethral discharge with an antibiogram, PCR studies of scrapings, and blood cultures for blood culture. The nature and severity of dysuric disorders in acute prostatitis is assessed using uroflowmetry.
Ultrasound of the prostate gland with moderate pain syndrome can be performed transrectally; in the case of a pronounced pain reaction - transabdominally. Echoscopically assesses the shape, size of the gland, the presence of focal or diffuse changes, the stage of acute prostatitis is established. The use of dopplerometry allows a detailed and differentiated assessment of the vascularization of the prostate.
When planning surgical tactics for destructive forms of acute prostatitis, it is advisable to perform CT or MRI of the pelvis.
Treatment of acute prostatitis
The leading role in the treatment of acute prostatitis belongs to etiotropic therapy. It is necessary to prescribe antimicrobial (antibacterial, antiviral, antitrichomonas, antimycotic) drugs as early as possible to suppress the reproduction of microorganisms in the gland and tissues of the urethra. In order to reduce spasms and painful urination, analgesics, antispasmodics, rectal suppositories with anesthesin or belladonna, and thermal microclysters are prescribed. In the complex therapy of acute prostatitis, NSAIDs, enzymes, immunomodulators, vitamins, infusions of solutions are used.
Physiotherapy for acute prostatitis is carried out after the acute symptoms subside. For the purpose of anti-inflammatory, anti-edema, analgesic action, improvement of microcirculation and local immunity, rectal electrophoresis, UHF therapy, microwave therapy, prostate massage are used. In acute prostatitis, bed rest, a sparing diet, and sexual rest are shown.
With urinary retention against the background of acute prostatitis, bladder catheterization is avoided, preferring trocar cystostomy. When abscessing the prostate gland, there is a need for a surgical aid for opening and draining the abscess cavity.
The cure of acute prostatitis is judged by the restoration of the structure of gland tissues and its functions, the normalization of the composition of prostate juice, the elimination of pathogens that caused inflammation from biological fluids.
Forecast and prevention
As a rule, timely and reasonable etiotropic therapy leads to relief of signs of acute prostatitis. Abscessing of the prostate or chronic inflammation occurs in advanced cases.
Prevention of acute prostatitis should include sanitation of infectious foci in the body, endovesical and endourethral manipulations in accordance with asepsis standards, timely treatment of STDs and urethritis, normalization of sexual life and physical activity.