Home >
Erectile Dysfunction >
Prostate screening what is it
Prostate screening what is it
You just need to remember about the prostate. Prostate Cancer Screening
If the topic did not imply an extreme degree of seriousness of the conversation, Prostate cancer could be called a pig in a poke. For a long time, measured in years, the disease can develop absolutely asymptomatically. Without pain, discomfort, any other manifestations of ill health. And then simultaneously "shoot" with all volleys at once. And, alas, often - to defeat.
It makes no sense to start being afraid ahead of time. But even less of it is to do nothing in a situation where you can find and neutralize the disease before it goes on the attack.
Be a man go to the doctor
Why is this needed?
The statistics of oncologists does not imply discrepancies: prostate cancer is a disease that is diagnosed more often than other oncopathologies. Even such common oncological diseases as lung cancer, colorectal cancer and breast cancer give way to the leader's place. Only about half of the cases of detected malignant tumors of the prostate have early stages of the disease, which, of course, affects the complexity of the treatment of the disease and its positive outcome. At the same time, if the disease is detected at an early stage, the probability of a complete recovery reaches 100%! Therefore, regular preventive examinations should justifiably be the first thing on the list of priorities for a modern and responsible man.
What is the point of screening?
Until now, the most common method for diagnosing prostate pathologies has been and remains the method of palpation during an internal examination by a urologist (digital rectal examination DRE). However, the traditional nature of the method in this case is not equivalent to its effectiveness. As a rule, malignant neoplasms detected in this way are already quite large. And an additional examination can reveal the spread of cancer cells to neighboring and distant organs.
An important element for the diagnosis of Prostate Cancer is also Transrectal ultrasound. But this method cannot be called unambiguously reliable and decisive for the diagnosis. Given the characteristics of a prostate tumor, almost every second case of prostate cancer remains "invisible" for ultrasound.
The most informative at present is a Blood test for PSA.
PSA - prostate-specific antigen - a protein that is produced exclusively by the prostate gland. Normally, its presence in the blood is permissible in low concentrations. Exceeding the threshold value of PSA may indicate pathological changes in the structure of the gland and the processes occurring in it.
Thus, screening for prostate cancer primarily involves a blood test for PSA in all men aged 50 to 65.
It is no coincidence that screening examinations are indicated for this particular age group. According to many years of confirmed data, malignant tumors of the prostate in men under 40 years of age are extremely rare. For another 10 years, the risk of pathology remains low. (The exception is men with a hereditary predisposition to prostate cancer.) But after 50 years, the likelihood of developing malignant neoplasms increases dramatically in all men, which is directly related to age-related changes in the body. At the same time, tumors are most often aggressive and, in the absence of timely and effective treatment, pose a direct threat to the patient's life. In men older than 70 years, if cancer has not been detected so far, there is no point in looking for it purposefully: as a rule, the tumor is so insignificant that it does not affect the overall well-being and quality of life. Or treatment at this age, the more radical, will not be of fundamental importance for the quality and duration of the patient's life.
Given these circumstances, a blood test for PSA with a frequency of 1 time in 2 years in men over 50 years old, as the first stage of preventive screening for early diagnosis of prostate cancer, most oncologists recognize as more than justified.
If the level of prostate-specific antigen exceeds the permissible limits, a second stage of examinations is provided. Namely: a systematic biopsy of the prostate gland under the control of transrectal ultrasound.
The upper limit of the norm is considered to be the content of PSA in the blood at a concentration of 4 ng / ml. However, in recent years, experts are inclined to reduce the threshold value of the PSA level to 2.5-3 ng / ml in men under the age of 55, believing that this can significantly increase the chances of diagnosing malignant tumors in the initial stage of development.
A biopsy is the only sure way to confirm or deny the presence of cancer cells. A systematic biopsy involves at least 6 punctures at the same time to exclude the disease.In some cases, their number can be significantly increased. The procedure is unpleasant, but for its implementation the most modern and effective painkillers are used to minimize pain and discomfort for the patient.
Scan is not to be missed
Actually, each reader can put a comma where he sees fit.
After all, it makes no sense to dissemble: the scientific community of oncologists has not yet come to a consensus on the unconditional benefits of screening for prostate cancer. The same level of PSA in the blood, for example, can be increased in a number of cases far from oncology. It is possible to detect an excess of the permissible concentration of the antigen with equal success, both with actual prostate cancer and with benign prostatic hyperplasia, and even after passionate intimacy on the eve of the analysis. It is for this reason that the presence of a malignant tumor is confirmed only in 30-50% of men with elevated PSA levels in the blood.
But here, perhaps, the most compelling argument for men should be a reminder: if there is at least a minimal chance to prevent the disease, it is foolish not to use it. At least for the sake of not turning the comma into a dot.
You just need to remember about the prostate. Prostate Cancer Screening
If the topic did not imply an extreme degree of seriousness of the conversation, prostate cancer could be called a pig in a poke. For a long time, measured in years, the disease can develop absolutely asymptomatically. Without pain, discomfort, any other manifestations of ill health. And then simultaneously "shoot" with all volleys at once. And, alas, often - to defeat.
It makes no sense to start being afraid ahead of time. But even less of it is to do nothing in a situation where you can find and neutralize the disease before it goes on the attack.
Be a man go to the doctor
Why is this needed?
The statistics of oncologists does not imply discrepancies: Prostate cancer is a disease that is diagnosed more often than other oncopathologies. Even such common oncological diseases as lung cancer, colorectal cancer and breast cancer give way to the leader's place. Only about half of the cases of detected malignant tumors of the prostate have early stages of the disease, which, of course, affects the complexity of the treatment of the disease and its positive outcome. At the same time, if the disease is detected at an early stage, the probability of a complete recovery reaches 100%! Therefore, regular preventive examinations should justifiably be the first thing on the list of priorities for a modern and responsible man.
What is the point of screening?
Until now, the most common method for diagnosing prostate pathologies has been and remains the method of palpation during an internal examination by a urologist (digital rectal examination DRE). However, the traditional nature of the method in this case is not equivalent to its effectiveness. As a rule, malignant neoplasms detected in this way are already quite large. And an additional examination can reveal the spread of cancer cells to neighboring and distant organs.
An important element for the diagnosis of prostate cancer is also transrectal ultrasound. But this method cannot be called unambiguously reliable and decisive for the diagnosis. Given the characteristics of a prostate tumor, almost every second case of prostate cancer remains "invisible" for ultrasound.
The most informative at present is a blood test for PSA.
PSA - prostate-specific antigen - a protein that is produced exclusively by the prostate gland. Normally, its presence in the blood is permissible in low concentrations. Exceeding the threshold value of PSA may indicate pathological changes in the structure of the gland and the processes occurring in it.
Thus, screening for prostate cancer primarily involves a blood test for PSA in all men aged 50 to 65.
It is no coincidence that screening examinations are indicated for this particular age group. According to many years of confirmed data, malignant tumors of the prostate in men under 40 years of age are extremely rare. For another 10 years, the risk of pathology remains low. (The exception is men with a hereditary predisposition to prostate cancer.) But after 50 years, the likelihood of developing malignant neoplasms increases dramatically in all men, which is directly related to age-related changes in the body. At the same time, tumors are most often aggressive and, in the absence of timely and effective treatment, pose a direct threat to the patient's life. In men older than 70 years, if cancer has not been detected so far, there is no point in looking for it purposefully: as a rule, the tumor is so insignificant that it does not affect the overall well-being and quality of life.Or treatment at this age, the more radical, will not be of fundamental importance for the quality and duration of the patient's life.
Given these circumstances, a blood test for PSA with a frequency of 1 time in 2 years in men over 50 years old, as the first stage of preventive screening for early diagnosis of prostate cancer, most oncologists recognize as more than justified.
If the level of prostate-specific antigen exceeds the permissible limits, a second stage of examinations is provided. Namely: a systematic biopsy of the prostate gland under the control of transrectal ultrasound.
The upper limit of the norm is considered to be the content of PSA in the blood at a concentration of 4 ng / ml. However, in recent years, experts are inclined to reduce the threshold value of the PSA level to 2.5-3 ng / ml in men under the age of 55, believing that this can significantly increase the chances of diagnosing malignant tumors in the initial stage of development.
A biopsy is the only sure way to confirm or deny the presence of cancer cells. A systematic biopsy involves at least 6 punctures at the same time to exclude the disease. In some cases, their number can be significantly increased. The procedure is unpleasant, but for its implementation the most modern and effective painkillers are used to minimize pain and discomfort for the patient.
Scan is not to be missed
Actually, each reader can put a comma where he sees fit.
After all, it makes no sense to dissemble: the scientific community of oncologists has not yet come to a consensus on the unconditional benefits of screening for prostate cancer. The same level of PSA in the blood, for example, can be increased in a number of cases far from oncology. It is possible to detect an excess of the permissible concentration of the antigen with equal success, both with actual prostate cancer and with benign prostatic hyperplasia, and even after passionate intimacy on the eve of the analysis. It is for this reason that the presence of a malignant tumor is confirmed only in 30-50% of men with elevated PSA levels in the blood.
But here, perhaps, the most compelling argument for men should be a reminder: if there is at least a minimal chance to prevent the disease, it is foolish not to use it. At least for the sake of not turning the comma into a dot.
Sergei Krasny. Deputy Director for Research, Republican Scientific and Practical Center for Oncology and Medical Radiology named after N.N. N. N
But it was a difficult and thorny 10 year journey. The main limitations were that screening examinations lead to overdiagnosis (i.e., the detection of minor tumors that did not manifest themselves in any way and did not entail any problems in the future), and, accordingly, to overtreatment. But in our country this issue is solved by the fact that we do not treat patients who have a minor tumor without a tendency to progress, but we observe it. In fact, this is how they do it all over the world. I can say with pride and joy that on April 17 of this year, justice prevailed. The American Urological Association acknowledged the effectiveness of prostate cancer screening and publicly apologized. Moreover, she decided to include screening for prostate cancer in her national standards for preventive examinations, and from May 1 they have already begun to operate in the United States. In other words, the whole world has now witnessed how a negative attitude towards screening examinations for early diagnosis of prostate cancer has changed to a positive one. Although they don't call it a screening, almost all American men do it for themselves. And in the US, stage 4 prostate cancer is less than 1%. Accordingly, we have more advanced forms of the disease. And we began to determine the level of PSA in the blood everywhere only recently. Nevertheless, even now we can confidently speak about the positive results of screening activities. Look: from 1999 to 2010, deaths from prostate cancer increased by 10% annually. And after 2011, it began to slowly but surely decrease by 2% every year, despite the fact that the incidence is growing. This is explained by the fact that with the introduction of screening, more cases of malignant neoplasms were detected in principle and more - at an early stage, when treatment guarantees complete recovery.
Sergei Krasny Deputy. Director for Research, Republican Scientific and Practical Center for Oncology and Medical Radiology named after N.N. N. N
At present, a PSA blood test can be taken at any clinic. Another thing is that not everywhere it is done for free. But it's a matter of time. And the cost is such that any person at any level of income can afford to do this analysis once every 2 years on a paid basis, if, I emphasize, it cannot yet be done at a polyclinic at the place of residence for free.As for biopsies, if an elevated PSA level in the blood is detected, they are performed simultaneously with the use of highly effective painkillers. The procedure can be performed in a day hospital. Hospitalization is not necessary.
Prostate screening what is it
Prostate cancer is a malignant neoplasm arising from the epithelium of the alveolar cell glands. Prostate cancer is responsible for almost 10% of tumor deaths in men and one of the leading causes of death in older patients.
Epidemiology
Prostate cancer tends to develop in older men and is the second leading cause of cancer deaths among men. Prostate cancer is a typical age-related disease. It does not cause any symptoms and, as a result, is not diagnosed for many years. At the same time, in fact, most men die with prostate cancer, not prostate cancer. Approximately 20% of men will develop prostate cancer during their lifetime, and only 3% will actually die from the disease.
Causes of prostate cancer
The main causes of prostate cancer include genetic predisposition, age-related hormonal changes, and nutrient imbalances. The presence of the XMRV virus is being considered as a possible additional cause.
Genetic factors. Scientists have calculated that about 9% of prostate cancer cases may be the result of a hereditary genetic predisposition. Approximately 15% of men with prostate cancer have a first-degree male relative (father or brother) with prostate cancer, compared to 8% in the general population. Medical scientists have identified a genetic alteration that increases the risk of developing prostate cancer. Researchers have identified four mutations in the "Hereditary Prostate Cancer 2" (HPC2) gene that predispose men to a greater risk of developing prostate cancer. Two of these mutations lead to a high risk of developing prostate cancer, while the other two mutations cause an average level of disease. Men who carry one of the two high risk mutations are 5 to 10 times more likely to develop prostate cancer, while men who carry one of the two moderate risk alterations are 1.5 to 3 times more likely to develop prostate cancer. higher than the general population.
External factors. To date, there is no clear understanding of why some people develop prostate cancer and others do not. Surprisingly, when people from areas with low rates of prostate cancer move to areas with higher levels of cancer, they are at higher risk of developing the disease, probably due to environmental changes, even though their genetic make-up has not changed. This suggests that environmental factors may play a larger role than genetic factors in the development of prostate cancer. Although the causes of prostate cancer remain controversial, scientists have identified several risk factors associated with prostate cancer.
Age. The scope of prostate cancer increases dramatically with age. Prostate cancer rarely appears in men under the age of 50. Prostate cancer is most common in men over the age of 55, and the median age of diagnosis is 70 years. The risk of prostate cancer increases exponentially after age 50. In fact, by the age of 60, 34% of men develop early signs of prostate cancer, and after 80 years, 70% of men already have this disease.
Diet. There is strong evidence that diet plays a role in the development of prostate cancer. Some studies show that prostate cancer is more prevalent in populations that eat a diet rich in animal fats and poor in certain nutrients. In fact, 15 out of 22 clinical studies found that eating a higher fat diet was associated with a higher risk of prostate cancer. One study showed that men who eat a high-fat diet have a 40% increased risk of developing prostate cancer.
Some studies conclude that diets rich in nutrients such as leukopene, vitamin E, and selenium may actually reduce the risk of prostate cancer. This supports the notion that diets deficient in these nutrients may increase the risk of prostate cancer. Certainly more research is needed to establish a clear link between diet and prostate cancer.
Hormones. To date, it has been determined that high testosterone levels can increase the risk of developing prostate cancer.
Race.The incidence of prostate cancer is highest among blacks, average among whites, and lowest among native Japanese and Native Americans. Black people are almost twice as likely to get prostate cancer as whites, and they are also twice as likely to die from the disease.
Prevention. Despite the fact that the distinct causes of prostate cancer have not been established, the existing presumptive etio-pathogenic factors must be identified and controlled.
Diet. Scientists have long evaluated the relationship between diet and all types of cancer, and intensive research into the relationship between diet and prostate cancer continues. A number of recent studies have shown that diets low in fat, leukopene, Vitamin E and selenium may play a role in preventing or at least slowing down the development of prostate cancer.
Leukopen is a carotenoid found primarily in tomatoes and tomato products. In 57 of 72 studies, leukopen was associated with a lower risk of prostate cancer. In one study, participants either received or did not receive leukopen supplementation prior to surgery. Only 33% of the leukopene supplement group developed cancer, compared with 75% of the control group. Moreover, the prostate-specific antigen (PSA) levels of the leukopene supplement group dropped by 20%, while the PSA concentration of the control group remained unchanged.
Vitamin E exists in two forms: alpha-tocopherol and gamma-tocopherol. Alpha tocopherol is the main form of vitamin E in drugs or supplements, while gamma tocopherol is the main form of vitamin E in the diet. Both of these substances are associated with a reduced risk of prostate cancer. One study focused on lung cancer suggested the benefit of vitamin E in reducing the risk of prostate cancer. The results showed that daily intake of 50mg of vitamin E supplementation over a 5-8 year course resulted in a 32% reduction in the incidence of prostate cancer. One pooled study examined the association between prostate cancer and three micronutrients: alpha-tocopherol, gamma-tocopherol, and selenium. The scientists used plasma and fingernail samples to measure the levels of three micronutrients in 117 men with prostate cancer and 233 men without cancer. The results demonstrated that these micronutrients are associated with a reduced risk of developing prostate cancer. The strongest association was found for gamma-tocopherol. The risk of prostate cancer for men with the highest levels of gamma-tocopherol was 5 times lower than for men with the lowest levels. The risk of developing prostate cancer decreased with increasing concentrations of gamma-tocopherol. Selenium and alpha-tocopherol are also associated with a lower risk of prostate cancer, but only when higher concentrations of gamma-tocopherol are present. Since alpha-tocopherol supplements can actually lower gamma-tocopherol levels, the researchers concluded that balancing the two could be an important factor in reducing the risk of prostate cancer.
Selenium is an essential element required for the formation and function of at least 13 proteins. Animal studies have shown that increasing the dietary intake of selenium can lead to a reduction in the incidence of certain types of cancer. A number of studies have found a link between increased selenium intake and a lower risk of developing prostate cancer. Two recent studies that compared groups taking selenium supplements with control groups showed a nearly 60% reduction in the risk of developing prostate cancer.
Influence of hormones. The association between lifetime testosterone levels and prostate cancer prompted scientists to investigate whether finasteride, a hormone inhibitor, could reduce the incidence of prostate cancer. A large placebo study is currently underway to evaluate finasteride as a chemopreventive agent for prostate cancer.
Screening and early diagnosis
Prostate cancer is the second leading cause of death among men. As with other types of cancer, early detection increases the chance of a cure; it is not yet clear whether screening for prostate cancer reduces the number of deaths from this disease. Often, after a diagnosis of prostate cancer, doctors and patients choose a course of "watchful waiting" rather than starting treatment.Despite controversy, it is still recommended that men have annual screening for the condition using digital rectal examination, prostate-specific antigen (PSA) blood testing, and transrectal ultrasound. It is now recommended that men begin PSA screening at age 50, and that African American men and men with a family history of prostate cancer begin annual screening at age 45.
Digital examination of the rectum. In a digital rectal examination, a doctor inserts a gloved finger into the rectum to assess tissue structure and size of the prostate. This method has been the most common prostate screening procedure for many years; however, whether this method is effective in reducing prostate cancer deaths remains to be determined.
Blood test for prostate-specific antigen (PSA). A simple blood test allows lab technicians to determine the levels of PSA, a protein produced and distributed by the prostate gland. High PSA levels may indicate the presence of prostate cancer cells or other non-cancerous prostate conditions.
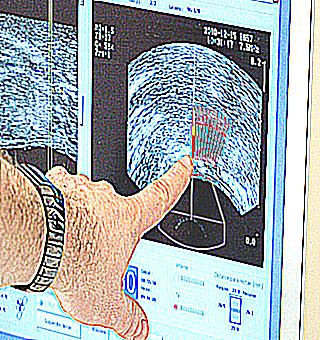
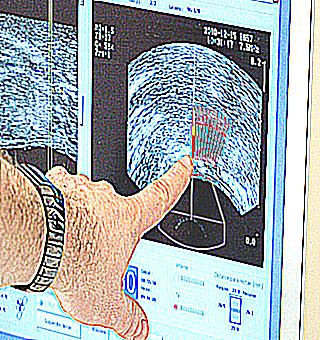
Transrectal ultrasound involves inserting a small probe into the rectum that emits high-frequency sound waves that bounce off the prostate and cause a visual echo. The computer uses the echo to create a picture, called a sonogram, which reveals abnormal areas. Scientists have yet to find out whether transrectal ultrasound is effective in reducing the number of deaths from prostate cancer.
While today's screening recommendations are standard, some research suggests that looking for predictors of prostate cancer earlier may be more effective. Recently, scientists conducted a study using special computer software to determine how many lives could be saved using a PSA test in each of seven different cases. Researchers have found that the most effective strategy is to start testing for PSA at age 40, repeat the test at 45 and 50, and test every two years thereafter.
Cancer screening is debatable when it remains to be seen whether the test actually saves lives. The controversy arises when it is unclear whether the benefits derived from screening may outweigh the risks of subsequent diagnostic tests and cancer treatments. For example: in a prostate cancer screening test, a PSA test can detect small malignant tumors that would never be a threat to life, but once detected, they will require treatment. This situation is called overdiagnosis, and it poses a danger to men in the form of complications from unnecessary treatment, such as surgery or radiation. Subsequent procedures used to diagnose prostate cancer (prostate biopsy) can also cause side effects, including bleeding and infection. Treatment for prostate cancer can cause incontinence (the inability to control the flow of urine) and erectile dysfunction (the level of erection is insufficient for sexual contact).
Strategy for improving screening and early detection
Researchers continue to develop and improve laboratory tests to improve the specificity of the PSA test. More specific PSA test results may help eliminate further invasive procedures, alleviate concerns, and reduce medical costs for patients with elevated PSA levels with a benign condition.
Prostate-specific antigens can be found in various forms in the blood, which can be difficult to interpret. Prostate-specific antigens can be associated with various molecules in the blood or exist as isolated "free" proteins. The a1 protease inhibitor is one of the specific proteins associated mainly with PSA in the blood. Previous studies have shown that the ratio of free PSA to total PSA increases the accuracy of prostate cancer detection. To further develop the specificity of PSA testing, scientists have recently developed a blood test that can detect the presence of a PSA-associated protease inhibitor a1.
Insulin-like growth factor (IGF-1) and insulin-like growth factor-binding protein 3 (IGF-SP-3) can help distinguish benign prostatic hyperplasia from prostate cancer. Elevated levels of IGF-1 and IGF-SP-3 in men with low to moderate PSA levels are warning signs of prostate cancer.The ratio of IGF-1 and IGF-SP-3 to free PSA is higher than the currently used free/total PSA ratio in the recognition of benign prostatic hyperplasia and prostate cancer.
Predictive genetic testing. Researchers have recently identified a genetic alteration that increases the risk of prostate cancer. There are 4 different alterations in the Hereditary Prostate Cancer 2 (HPC2) gene, the presence of which indicates an average or high risk of prostate cancer in men. Although scientists do not yet understand how NRP2 alterations affect the subsequent development of prostate cancer, they continue to investigate the properties and characteristics of this gene. Since questions about the dynamics of this gene are still open, more accurate information could contribute to the development of predictive genetic testing and perhaps even the creation of new drugs for prostate cancer that will be directed exclusively at this genetic alteration. While the identification of HRP2 is promising, more research is needed before testing for HRP2 becomes available in clinical practice.
Since 1994, the relationship between the GSTP1 gene and prostate cancer has been studied. In their recent clinical study, scientists evaluated the accuracy of GSTP1 gene methylation levels in predicting the presence of prostate cancer. The researchers examined surgically removed prostate tissue from 69 patients with localized prostate cancer and 31 patients with benign prostatic hyperplasia. Of the 69 patients with localized prostate cancer, 28 also had precancerous tissue, which was studied. The mean ratio of methylated GSTP1 genes to control gene in other tissue samples was 0 for tissue with benign prostatic hyperplasia, 1.4 for precancerous tissue, and 250.8 for clinically localized prostate cancer. The scientists also analyzed the effectiveness of measuring GSTP1 gene methylation in diagnosing prostate cancer in small biopsy specimens. For this clinical study, the ratio of the methylated GSTP1 gene to the control gene was measured in small biopsy specimens taken from 21 patients with high PSA levels. Of all patients, 10 patients were correctly diagnosed as having no prostate cancer, and 10 out of 11 were correctly diagnosed with prostate cancer using the GSPT1 ratio. These results are encouraging and show that the measurement of GSTP1 methylation can be used to improve the accuracy of early stage prostate cancer detection.
Microbubble ultrasound. New advances in ultrasound include the use of color Doppler imaging in combination with microbubble contrast, which allows doctors to more effectively determine the presence and exact position of a mass in the prostate itself. Microbubbles are tiny bubbles of gas that can pass through small blood vessels without causing any harm. Bubbles enhance the image by increasing the intensity of the background scattering signal. Due to the fact that blood vessels and blood flow predominate more in cancerous tissues than in normal tissues, microbubbles are concentrated in cancerous tissues, which is displayed on the ultrasound picture. Microbubble Doppler data allows doctors to more accurately determine where to take a biopsy. Recently, scientists have compared doppler ultrasound with microbubble contrast agent and conventional ultrasonography. Patients (84 males) participating in this study were first examined using microbubble Doppler sonography, then they underwent 5 biopsies. The patients then underwent standard (black and white) ultrasonography and 10 biopsies. Later, the accuracy of the biopsies could be compared for the same patient. The detection rate for prostate cancer was 27% for Doppler biopsies compared with 20% for conventional ultrasonography. The overall baseline detection rate for prostate cancer by biopsy was 13% for Doppler biopsies compared with 4.9% for conventional ultrasonography. These results indicate that the use of Doppler techniques in conjunction with microbubble contrast may enable clinicians to more accurately determine the optimal biopsy site. This will result in fewer biopsies than conventional ultrasonography and an increased rate of cancer detection. Moreover, costs can be reduced by almost 50%.
So every year, starting at age 50, men with a future life expectancy of at least 10 years should have a blood test for prostate-specific antigen (PSA) and a digital rectal exam ( AT).Men from the high-risk group (African Americans, as well as patients with one or more first-degree relatives of the father, brothers diagnosed before the age of 65 with prostate pathology) should begin to undergo examinations at 45 years of age. Men at even higher risk who have several first-degree relatives with the condition at an early age in their family may begin screening at age 40. Depending on the results of the first test, further diagnostic procedures may be delayed until the age of 45.
All men should be given information about the benefits, limitations and dangers of early detection and treatment of prostate cancer, as well as the concerns that exist. This will allow them to make a decision to conduct this survey based on complete and reliable information.
It is also necessary to perform an examination of those men who ask the doctor to make a decision on their own. The examination should not be hindered. In addition, it is always necessary to offer this examination.
MRI has also recently been used to screen for prostate cancer.
There are several treatment options for the disease: observation with symptomatic treatment, radical prostatectomy, radiation therapy and brachytherapy.
The prognosis of the disease depends on the stage of the process. The earlier treatment is started, the higher the likelihood of a favorable outcome. In the early stages, with adequate treatment, the prognosis is conditionally favorable, the ability to work is fully restored. In the later stages, the prognosis is certainly unfavorable, the disease is fatal.